Tuesday 30 April 2019
Monday 29 April 2019
Health Consumers Are Now Amazon-Primed for Healthcare – HealthConsuming Explains, Part 2
 As patients now assume the role of health consumer, they rationally expect retail-level experiences with greater first-dollar payment for health insurance, health care services and medical products like prescription drugs.
As patients now assume the role of health consumer, they rationally expect retail-level experiences with greater first-dollar payment for health insurance, health care services and medical products like prescription drugs.
Consumers know what good retail looks and feels like, and are focusing that experiential lens on health care, Aflac found when their Workforces Survey polled Americans on what they’d like their health insurance shopping process to feel like. One in two people said, “like Amazon,” and another 20% of folks said, “like retail.”
Chapter 3 of HealthConsuming is titled, “How Amazon Has Primed Health Consumers,” and explains this re-shaping of patient expectations. Here’s one of my paragraphs from the chapter, noting that, “Health consumers are hungry for Amazon’s brand of transparency, convenience, and streamlined interactions for medical care. The Amazon Prime-ing of the U.S. consumer has raised peoples’ expectations of what health care services could be: personalized, customized, anticipatory, immediate or on-schedule, and convenient – where we live, work, play, pray, learn and even drive.”
 People trust Amazon for daily retail experiences. The bar chart from research by Market Strategies shows that a plurality of consumers also trusts Amazon to try on for healthcare products and services. The company has been multi-tasking a broad range of tactics throughout the health care ecosystem. Every publicly traded market segment Amazon has touched has had moments of shattering stock prices.
People trust Amazon for daily retail experiences. The bar chart from research by Market Strategies shows that a plurality of consumers also trusts Amazon to try on for healthcare products and services. The company has been multi-tasking a broad range of tactics throughout the health care ecosystem. Every publicly traded market segment Amazon has touched has had moments of shattering stock prices.
In the past couple of months, Amazon announced many health-related plans and developments, including:
- Accepting medical and health savings accounts (HSAs) to pay for consumer health products like over-the-counter drugs.
- Developing Alexa-skills that are HIPAA-compliant to bolster users’ personal health information privacy collaborating with Atrium Health, Boston Children’s Hospital, CIGNA, Express Scripts, Livongo Health, and Providence St. Joseph Health. In each instance, the developer organizations see voice as the next frontier for conveniently accessing health care services.
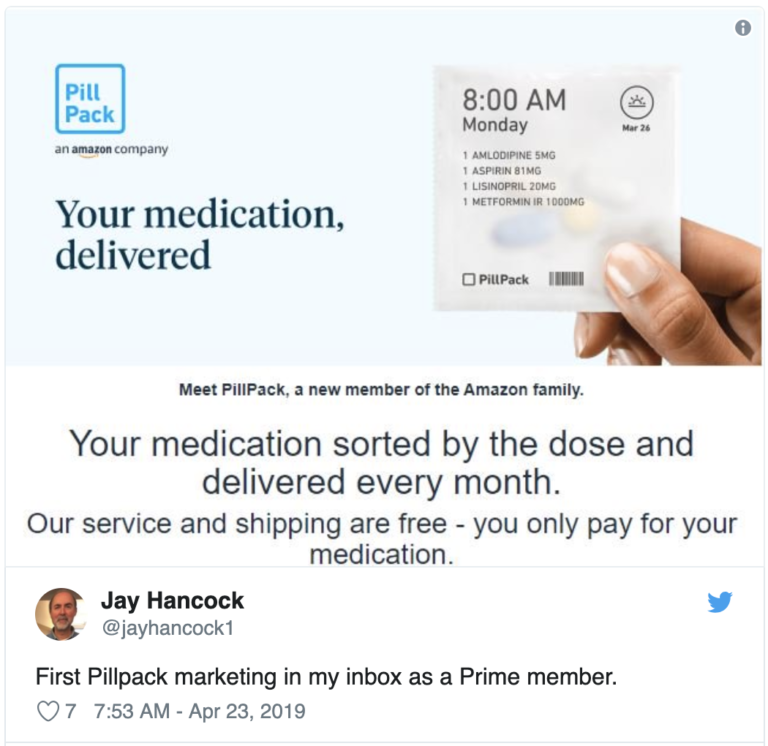
- Marketing PillPack, the subscription prescription drug service, to consumers, with the subtext that this may be Amazon Prime-eligible.
- Naming the Amazon-JPM-Berkshire Hathaway venture in health care organization “Haven,” and announcing plans to hire staff in New York City.
- Expanding Alexa skills to join the growing tele-mental health supply side.
- Launching a private label skin care line, Belei, covered in Allure magazine here. (The name is a combo of “believe” and “beauty,” and the disruptive ingredient with this beauty brand is that no product exceeds $40.
 Jim Cramer of CNBC’s Mad Money has been studying up on digital health, recently recommending that Apple buy Epic, the health IT behemoth. (See more on that recommendation, and subsequent social media frenzy, here on Health Populi). This month, he recommended that companies and investors need to study Amazon as a sort of “Death Star” in how the company re-defines industries — whether movies or music, retail or….health care.
Jim Cramer of CNBC’s Mad Money has been studying up on digital health, recently recommending that Apple buy Epic, the health IT behemoth. (See more on that recommendation, and subsequent social media frenzy, here on Health Populi). This month, he recommended that companies and investors need to study Amazon as a sort of “Death Star” in how the company re-defines industries — whether movies or music, retail or….health care.
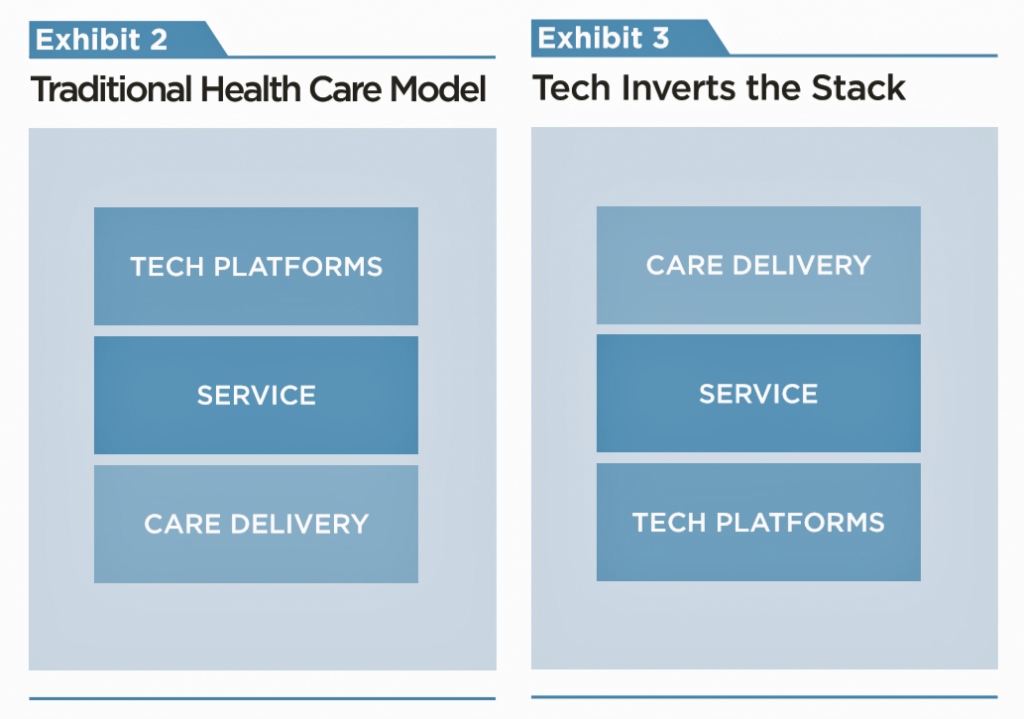
For health consumers, Amazon’s multi-tasking efforts are re-shaping health care service delivery and channeling.
Most importantly, in this immediate moment, Amazon has re-shaped patients as health consumers — our expectations for what is possible in health care delivery, price transparency, peer-to-peer advice, and convenience.
In tomorrow’s Health Populi, we’ll dive into a third key theme in HealthConsuming: that’s what we know-we-know about ZIP codes, food, deaths of despair, and the social determinants of health. Where we live portends how healthy we are…and why spending on social care is key to addressing health and longer life spans…the personal health version of surviving a death star.
On Thursday, my post will raise Amazon’s role in health/care again, looking more deeply into the promise of digital health and the perils of privacy for health, retail, and other personal data. Amazon isn’t just about convenient delivery of health care “things.” It’s about the data generated by those transactions, which help to construct profiles on you and me. Using such profiles can be very helpful for health, if that’s the intent of the data-miner. But as the Financial Times pointed out today in an op-ed written by its editorial board, “Platform companies from Amazon to Google to Apple are getting deep into the healthcare field, allowing us to do everything from communicate with doctors to check on prescriptions. The privacy implications are troubling….they are [also] surveilling consumers at the same time — gathering, analysing and, in many cases, selling sensitive data. In many countries, personal healthcare data are subject to strict regulation. In the US, the Health Insurance Portability and Accountability Act (HIPAA) imposes criminal and civil penalties for breaching confidentiality of healthcare data. But the rules apply only to entities covered by HIPAA such as healthcare plans and providers, or clearing houses that process healthcare claims.”
Stay tuned to tomorrow’s post, on social determinants of health and social spending. By Friday, the dots will converge on the topic of morphing from health consumers to health citizens.
The post Health Consumers Are Now Amazon-Primed for Healthcare – HealthConsuming Explains, Part 2 appeared first on HealthPopuli.com.
Health Consumers Are Now Amazon-Primed for Healthcare – HealthConsuming Explains, Part 2 posted first on http://dentistfortworth.blogspot.com
Sedation Dentistry – Your Ultimate Guide
There are a number of reasons that adults—grown adults—avoid trips to the dentist.
According to the American Dental Association, over 17% of people admit they avoid going to the dentist due to anxiety. And this “demotivator” is right behind the very real inability to pay for dental services that leaves millions of patients avoiding appointments each year. There are still others who have special needs or who are facing complex dental procedures, which result in fear or apprehension when faced with a visit to the dentist.
If you or a family member—even children—can identify with any of these issues, then it might be worthwhile to consider if sedation dentistry is right for you. Don’t let the word “sedation” cause more anxiety, though! This option is a safe and gentle for almost all ages. Keep reading as we break down the types of sedation available as well as the groups of patients who may be best served by sedation dentistry.
What is sedation dentistry?
Sedation dentistry offers patients relief from anxiety and pain and ensures a pain–free procedure—many times without any memory of the appointment. While many complex procedures are performed with some form of anesthesia, it is possible for general cleaning to also take place under sedation for those patients who suffer from severe anxiety.
There are several levels of sedation we use, all depending on the complexity of the procedure. The American Dental Association, in conjunction with state guidelines, offers a set of best practices for the administration of local anesthesia, sedation, and general anesthesia. Your dentist will decide which level of sedation is best for you. Below is a breakdown of the varying types of anesthesia typically used:
- Nitrous oxide: This is the most common form of sedation, and while it doesn’t put you all the way to sleep, it can reduce anxiety during a dental procedure. More commonly known as laughing gas, nitrous oxide is combined with oxygen and administered through a mask that is placed over the nose. This sedative can wear off quickly, so your dentist will actively monitor your anxiety and pain levels throughout the procedure.
Another benefit of nitrous oxide is that you can drive yourself home after the procedure. This is a good option for your bi-annual appointment or for less invasive procedures.
- Oral sedation: Also known as enteral sedation, this option encompasses all types of sedation that come in pill or liquid form. This option is helpful for easing nerves prior to getting to your appointment. Many times, this option is used in conjunction with nitrous oxide. Typically, the prescribed pill is Halcion, which is a member of the same drug family as Valium and is taken about an hour before the procedure.
This pill will make you drowsy, though you’ll still be awake. A larger dose may be given to produce moderate sedation. Depending on the dose, you might fall asleep during the procedure.
- IV sedation: This type of sedation will put you in a deeper level of sedation, rendering you totally unaware of what is happening around you. While technically still awake, most patients report no memory of what happened during a procedure.
And, just like with nitrous oxide, your dentist will continuously monitor your level of sedation through the procedure and adjust it as necessary.
- General anesthesia: This is the deepest level of sedation and should only be performed by highly–qualified practitioners in appropriate settings. This type of sedation is used most frequently for patients with special needs or who require the most complex dental treatments.
Who’s eligible for sedation dentistry?
Anxious patients
As mentioned, dental anxiety is a highly present issue among adults. If you suffer from dental anxiety, but have trouble articulating your fears with your dentist, your provider might choose to utilize the Corah’s Dental Anxiety Scale. Developed in 1969, this four question survey allows patients to choose from five answers. Each answer corresponds with numerical score. The total score allows the dentist to determine how anxious you are about the appointment.
Another assessment tool is the Modified Dental Anxiety Scale. This survey consists of five questions, each with a five-category rating scale, ranging from “not anxious” to “extremely anxious.” One difference in this survey is that it has an extra item about the respondent’s anxiety to a local anesthetic injection as well as the dental procedure itself.
Based on the results of the survey, your dentist may recommend sedation as part of your treatment.
Special needs patients
The special needs population is diverse and has a wide range of dental needs. Due to this, the reasons for the use of sedation dentistry are equally varied. Not only does this influence the type of anesthesia used, it also makes an impact on how the anesthesia is introduced.
For instance, special needs patients may have physical limitations as well as intellectual disabilities, each of which are vital components that are taken into consideration. One common example of special needs dentistry is serving those with autism. Since the dentist’s office can present an array of sensory challenges such as new tastes, smells and textures, sedation can offer a calmer experience. If you or your child have special needs, have a conversation with your dentist ahead of time to discuss options to make the patient most comfortable.
Complex procedures
Finally, some dental procedures can take several hours to complete. Since many patients would prefer to be in the chair for the least amount of time possible, they choose to break these procedures into multiple visits. However, sedation density allows patients to calmly complete complex procedures in a single visit. For example, patients who need extensive rebuilding procedures or multiple cavities filled at one time may be good candidates for sedation dentistry.
Are there risks to sedation dentistry?
As with any procedure, it’s important to discuss with your dentist if you are a good candidate for sedation dentistry. For those with sleep apnea or adverse reactions to anesthesia, it’s important to discuss your medical history with your dentist prior to any procedure.
Finally, everyone reacts differently to the different medications used for sedation. This includes how much is needed for complete sedation as well as any adverse feelings upon “coming to.” If you are concerned about how you may react, make sure to ask your dentist prior to your appointment.
Sedation dentistry has the ability to transform the practice of dentistry for those that avoid it due to anxiety or fear of pain. If you are interested in what Dr. Ku’s office has to offer, give us a call today!
The post Sedation Dentistry – Your Ultimate Guide appeared first on Fort Worth Dentist | 7th Street District | H. Peter Ku, D.D.S. PA.
Sedation Dentistry – Your Ultimate Guide posted first on http://dentistfortworth.blogspot.com
Patients Become Healthcare Payors, Now Consumers – HealthConsuming Explains, Part 1
We Are All Health Consumers Now. That’s the title of the first chapter of my new book, HealthConsuming: From Health Consumer to Health Citizen. I start this chapter quoting President Ronald Reagan in 1983, who recognized that health care costs were growing at three times the rate of inflation during the first term of his Presidency.
It’s déjà vu in health care all over again, but 35 years later, it’s the patient now facing sticker-shock with first dollar payments in high-deductible health plans, six-figure prices on specialty drugs to treat cancers, and a poor return-on-investment for personal health spending.
Thus begins my journey, with you the reader, ex plaining how patients-as-payors, now nudged into the role of consumer, could morph into health citizens: with rights to health care, bolstered privacy protections; more care in the community and at home to boost quality and safety and reduce costs, and, more opportunity and responsibility for self-care.
plaining how patients-as-payors, now nudged into the role of consumer, could morph into health citizens: with rights to health care, bolstered privacy protections; more care in the community and at home to boost quality and safety and reduce costs, and, more opportunity and responsibility for self-care.
In the Health Populi blog this week, I’ll take each weekday to explain one part of this story: the patient-as-payor, now consumer; how Amazon has primed health consumers, with informed retail service expectations; what we know about ZIP codes, food, deaths of despair and the social determinants for health; the promise of digital health and perils of privacy; and finally, whether health consumers in the U.S. can/will emerge as health citizens. All of these themes are backed up by 519 endnotes in the back of the book, as I connect the dots of the rich evidence base for telling this story.
 First, let’s explore the scenario-reality of the patient-as-payor, now consumer. This is a contentious issue, debated from my admired economist-guru Paul Krugman in the New York Times in 2011 when he contended that patients weren’t consumers; to last week in Medscape, when bioethicist, and another admired thinker, Dr. Art Caplan, echoed the same.
First, let’s explore the scenario-reality of the patient-as-payor, now consumer. This is a contentious issue, debated from my admired economist-guru Paul Krugman in the New York Times in 2011 when he contended that patients weren’t consumers; to last week in Medscape, when bioethicist, and another admired thinker, Dr. Art Caplan, echoed the same.
Health Affairs covered this topic, too, last month, which I discussed here in Health Populi.
The data, though, demonstrate the growing adoption of high-deductible health plans, co-payments and coinsurance for health plan members. When people face first-dollar out-of-pocket spending, they are assigned the role of consumer in choosing to spend that money out of household budgets. The latest research from the Bureau of Labor statistics is that on a median household basis, 20% of spending goes to healthcare.
That’s the immediate situation for real people facing real diagnoses, today and tomorrow, in 2019.
“Today’s high deductibles are tomorrow’s bad debt,” a Moody’s analyst recently wrote. This starts the theme of the second chapter — The Patient is the Payor.
 Health care costs stress out people at all income levels in the U.S., according to the American Psychological Association‘s annual study on Stress in America. And this goes, too, for people both uninsured and insured. This isn’t a new-new finding: even families earning over $90,000 a year cited health care costs as their #1 pocketbook issue, a Kaiser Family Foundation study learned in 2015.
Health care costs stress out people at all income levels in the U.S., according to the American Psychological Association‘s annual study on Stress in America. And this goes, too, for people both uninsured and insured. This isn’t a new-new finding: even families earning over $90,000 a year cited health care costs as their #1 pocketbook issue, a Kaiser Family Foundation study learned in 2015.
This sets the stage for understanding how patients, now consumers, paying more directly for health care in deductibles and OOP expenses are, justifiably, expecting greater service, experiences, value and return-on-investment from th ehealth care industry. Welcome to the next section of HealthConsuming, the Amazon-Prime-ing of health consumers, in tomorrow’s Health Populi blog,
The post Patients Become Healthcare Payors, Now Consumers – HealthConsuming Explains, Part 1 appeared first on HealthPopuli.com.
Patients Become Healthcare Payors, Now Consumers – HealthConsuming Explains, Part 1 posted first on http://dentistfortworth.blogspot.com
Will you be able to afford senior housing when you get old?
As the U.S. ages, more and more individuals have chronic conditions or functional limitations which may at some point require senior housing, such as independent or assisted living facilities and nursing homes. The question is, will individuals be able to afford this type of housing? According to a paper by Pearson et al. (2019), the answer for most people the answer will be ‘no’.
…by 2029 there will be 14.4 million middle-income seniors, 60 percent of whom will have mobility limitations and 20 percent of whom will have high health care and functional needs. While many of these seniors will likely need the level of care provided in seniors housing, we project that 54 percent of seniors will not have sufficient financial resources to pay for it.
The authors come to this conclusion by projecting future chronic conditions, functional limitations and income levels trends derived from the Health and Retirement Survey (HRS). Note that assisted living costs about $44,400 on average per year and costs have risen over time. Perhaps surprisingly, it may not be the poor who will not be able to afford senior housing, but instead middle income individuals may the ones get squeezed.
Seniors housing operators and investors have largely focused on the upper end of the income distribution. For lower-income people, state and local programs provide housing and care services via means-tested programs such as Medicaid… Although some middle-income people are living in seniors housing, the industry has not primarily focused on this cohort. This income group is generally too wealthy to qualify for public means-tested programs, yet not wealthy enough to pay the costs at many seniors housing communities for a sustained period of time.
The decrease in employer use of pensions and under-saving by employees through 401(k) options, make this issue even more acute.
Source:
- Caroline F. Pearson, Charlene C. Quinn, Sai Loganathan, A. Rupa Datta, Beth Burnham Mace, and David C. Grabowski. The Forgotten Middle: Many Middle-Income Seniors Will Have Insufficient Resources For Housing And Health Care Health Affairs.
Will you be able to afford senior housing when you get old? posted first on http://dentistfortworth.blogspot.com
Friday 26 April 2019
Across All Political Parties, Likely Voters Over 50 Favor Cutting Prescription Drug Prices
People over 50 in the U.S. that are likely to vote in the 2020 Presidential election are keenly interested in lowering the cost of prescription drugs, according to a survey conducted by AARP in February and March 2019.
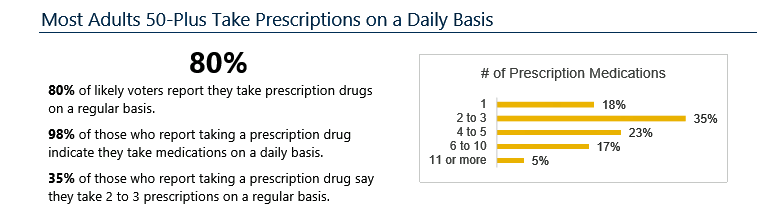 Most people over 50 take prescription drugs daily; one-third take two or three Rx’s regularly, and one in five older people take six or more prescription medicines regularly.
Most people over 50 take prescription drugs daily; one-third take two or three Rx’s regularly, and one in five older people take six or more prescription medicines regularly.
Thus, prescription drugs are part of most older Americans’ daily life-flows and household spending considerations.
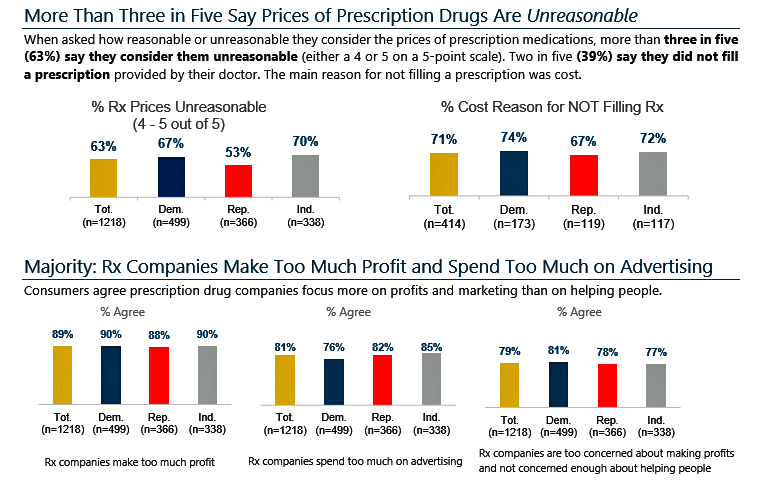 About two-thirds of older people who are likely to vote say that Rx prices are “unreasonable,” including 67% of Democrats, 70% of Independents, and 53% of Republicans.
About two-thirds of older people who are likely to vote say that Rx prices are “unreasonable,” including 67% of Democrats, 70% of Independents, and 53% of Republicans.
Strikingly, 71% of likely older voters told the AARP that cost was a reason for not filling a prescription drug. This medicine self-rationing behavior due to cost is common among a majority of older voters across party-identification: 74% of Democrats, 67% of Republicans and 72% of Independents.
Older voters are making trade-offs to be able to buy Rx medicines: currently, one in four older people has delayed getting a prescription filled as they didn’t have enough cash to do so; and, one in four older people took less medicine than prescription to make it last longer.
Looking to the future, 4 in ten older voters told AARP they may have to cut back on necessities like food, fuel and utilities to afford an Rx drug, or delay filling the prescription due to lack of available funds to pay for it. Four in ten older voters would look to purchase an over-the-counter medicine to treat a condition.
It’s a rational response, then, that 9 in 10 older voters agree that pharmaceutical companies “make too much profits,” once again consistent — equally felt — by older voters across all three political parties, shown in the second bar chart.
Furthermore, 8 in 10 older U.S. voters contend that Rx companies spend too much on advertising, and that they are “too concerned about making profits, not concerned enough about helping people.”
85% of older voters also believe that U.S. consumers pay more for prescription drugs compared with peers in other wealthy countries.
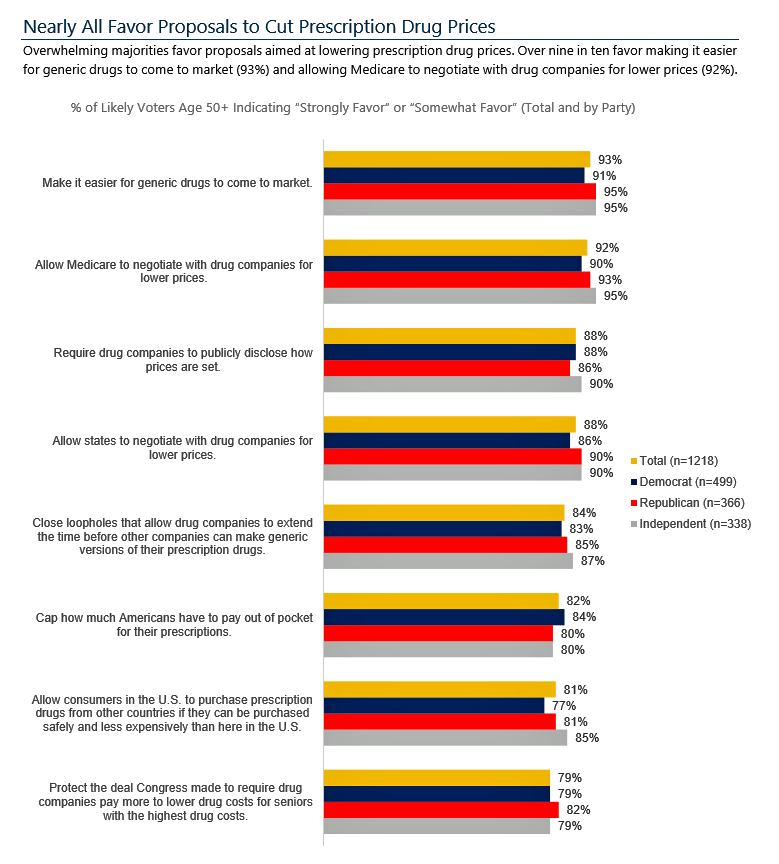 Health Populi’s Hot Points: The third chart illustrates that pharma pricing is a unifying force across older voters across the three political parties. Fully 9 in 10 people over 50 who intend to vote favor a wide range of prescription drug price lowering strategies such as faster generic approvals, allowing Federal Medicare and State governments to negotiate for lower prices as Americans’ fellow patients in other countries benefit from, and allowing U.S. consumers to import cheaper prescription drugs from other countries.
Health Populi’s Hot Points: The third chart illustrates that pharma pricing is a unifying force across older voters across the three political parties. Fully 9 in 10 people over 50 who intend to vote favor a wide range of prescription drug price lowering strategies such as faster generic approvals, allowing Federal Medicare and State governments to negotiate for lower prices as Americans’ fellow patients in other countries benefit from, and allowing U.S. consumers to import cheaper prescription drugs from other countries.
While deep understanding of how U.S. health care “works” eludes so many Americans, one common area of health system literacy is older patients’ comprehension of prescription drug pricing at the point of person-and-purchase. The AARP study findings confirm the premise in my book, HealthConsuming: From Health Consumer to Health Citizens — that the patient is now a consumer and payor, looking for value at the N of 1 — for themselves and their families. There’s an opportunity for pharma companies, health plans, and Payors (employers, unions, and government plans) to surround health consumers with the mantra of “value around the pill.” Collaborations can be struck to help people help themselves when it comes to self-care and engaging in making health. Yes, there’s the issue of price which the President and Secretary of HHS continue to discuss. But there is much the private sector can do to address costs, transparency, and value-added services to re-gain patient trust and health engagement.
Between “now” and the 2020 Presidential election, it’s clear this issue will be top-of-mind for likely voters over 50 years of age: the biggest health consumers of prescription drugs.
The post Across All Political Parties, Likely Voters Over 50 Favor Cutting Prescription Drug Prices appeared first on HealthPopuli.com.
Across All Political Parties, Likely Voters Over 50 Favor Cutting Prescription Drug Prices posted first on http://dentistfortworth.blogspot.com
Friday Links
- How digital medicine saved his life.
- What is the key ingredient for shared decision making?
- Singaporean health system.
- Medicare exploring global budgets for primary care.
- Bucks sweep.
Friday Links posted first on http://dentistfortworth.blogspot.com
Thursday 25 April 2019
6 Strategies for Demonstrating the Value of Gene Therapy to Payers
An interesting white paper on how to demonstrated value to payers when examining gene therapies has hit the presses. My colleagues Jeremy Schafer, PhD, and Alexander Grosvenor, PhD have written a guide to help you:
- Understand the disparities between payer and manufacturer expectations for long-term outcomes
- Determine which elements of treatment are included in the product cost
- Shift the dialogue from short-term results to long-term savings
- Gain 6 strategies to craft a compelling value story for a gene therapy
You can download the paper anytime. An excerpt is below.
Due to the uncertainty surrounding long-term outcomes, there may be a significant disparity between a payer’s expectations for long-term outcomes and the manufacturer’s expectations. The example of Glybera—and its discontinuation in the EU market—highlights the critical importance of a robust demonstration of benefit. Health technology assessments (HTAs) for Glybera were performed by the pricing and reimbursement agencies in France and Germany, and both agencies found insufficient or unquantifiable benefit to justify reimbursement.
6 Strategies for Demonstrating the Value of Gene Therapy to Payers posted first on http://dentistfortworth.blogspot.com
Wednesday 24 April 2019
A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank
People define their personal health and well-being broadly, well beyond physical health. Mental wellness, physical appearance, social connections, and financial wellness all add into our self-health definitions.
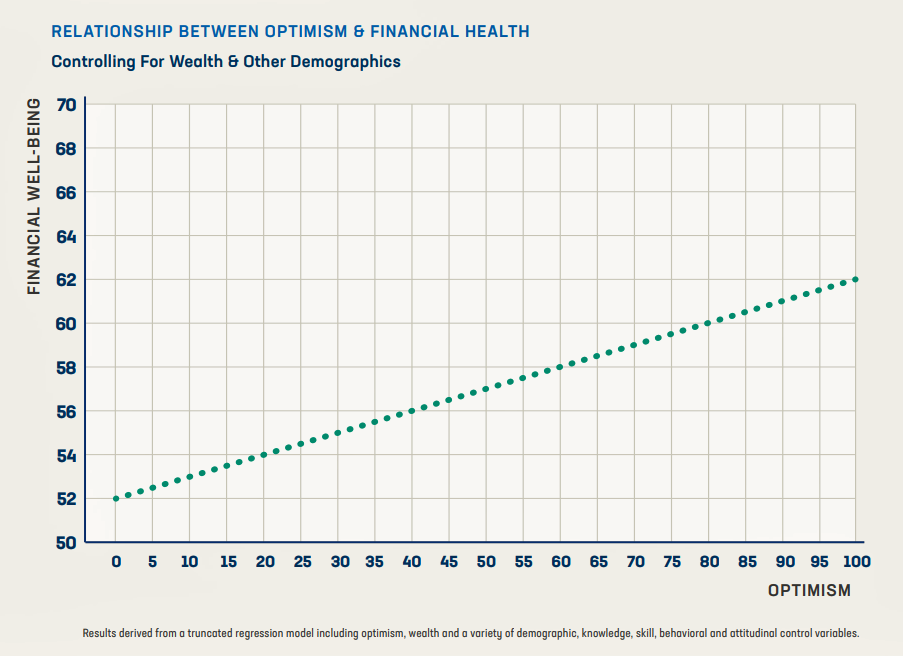
 Mind Over Money is a consumer study conducted by Frost Bank, working with FleischmanHillard, connecting the dots between optimism and financial health.
Mind Over Money is a consumer study conducted by Frost Bank, working with FleischmanHillard, connecting the dots between optimism and financial health.
The top-line of the study is that people who are optimists have roughly two-thirds fewer days of financial stress per year than pessimists. Put another way, pessimists stress about finances 62% of the year, shown in the first chart from the study.
This translates into 62% of optimists having better financial health, seven times greater than pessimists at 9%.
In a regression analysis, the study showed a significant relationship between optimism and
better financial health: a 1-point increase in optimism was associated with a 0.1-point increase in financial well-being. Optimism was associated with an increase in financial well-being of up to 10 points. This straight-line relationship is illustrated in the second graph showing that greater optimism, controlling for wealth and other demographics, is related to greater financial well-being.
 The study identified several other data points that paint the financially unwell profile of Americans:
The study identified several other data points that paint the financially unwell profile of Americans:
- Six in ten people say finances control their lives at least sometimes
- On average, Americans have five months of financial stress annually
- Nearly 9 in 10 Americans have experience at least one financial setback.
The survey polled 2,002 U.S. adults 18 and over in September 2018 in English and Spanish.
Health Populi’s Hot Points: “By believing that life’s challenges are temporary rather than permanent, people can feel inspired to take meaningful steps to improvement,” Michelle Gielan, a psychologist with whom Frost collaborated for the study, asserts in the report. Optimism can be a catalyst for better physical and emotional health, Michelle adds, noting that Americans want more optimism in their lives.
Let me call out the front half of the first sentence here:
“By believing that life’s challenges are temporary rather than permanent…”
Millions of Americans feel health in-secure, both those with insurance who perceive they are under-insured and cannot afford their premiums or co-payments, and those who are uninsured.
That perception of healthcare insecurity has a negative impact on financial wellness and health status.
I discuss this phenomenon in my new book, HealthConsuming: From Health Consumer to Health Citizen. In Chapter 2, titled “The Patient Is the Payor,” you’ll read the introductory quote from a Moody’s analyst observing that, “Today’s high deductibles are tomorrow’s bad debt.”
This week, Health Affairs published an essay on The Challenges of High-Deductible Plans For Chronically Ill People. The authors note that, “There is a significant number of Americans who cannot simply elect to limit their use of health services or can do so only by risking severe consequences. For the 60 percent of Americans living with at least one chronic condition, high deductibles present precarious financial conditions that recur every January 1. As the National Center for Health Statistics has reported, people with HDHPs are far more likely than those with traditional health plans to forgo or delay medical care or to be in a household that is having difficulty paying medical bills.” The piece presents scenarios for patients dealing with cancer, auto-immune disease, and epilepsy.
For people enrolled in high deductible health plans dealing with chronic conditions, one-half felt financial stress due to health care costs versus 21% of people enrolled in conventional health plans.
High deductible health plan designs continue to grow and mainstream in both commercially-insured populations for people receiving employer-sponsored plans, as well as for folks enrolling in public sector and marketplace plans. In thinking through health care reform futures and how people live daily lives, in health and illness, we should be mindful of bundling in financial wellness into our visions for making healthcare better in America.
The post A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank appeared first on HealthPopuli.com.
A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank posted first on http://dentistfortworth.blogspot.com
Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical
The 2019 Edelman Trust Barometer measured the biggest gap in trust for the healthcare industry between the U.S. “informed public” and the mass population.
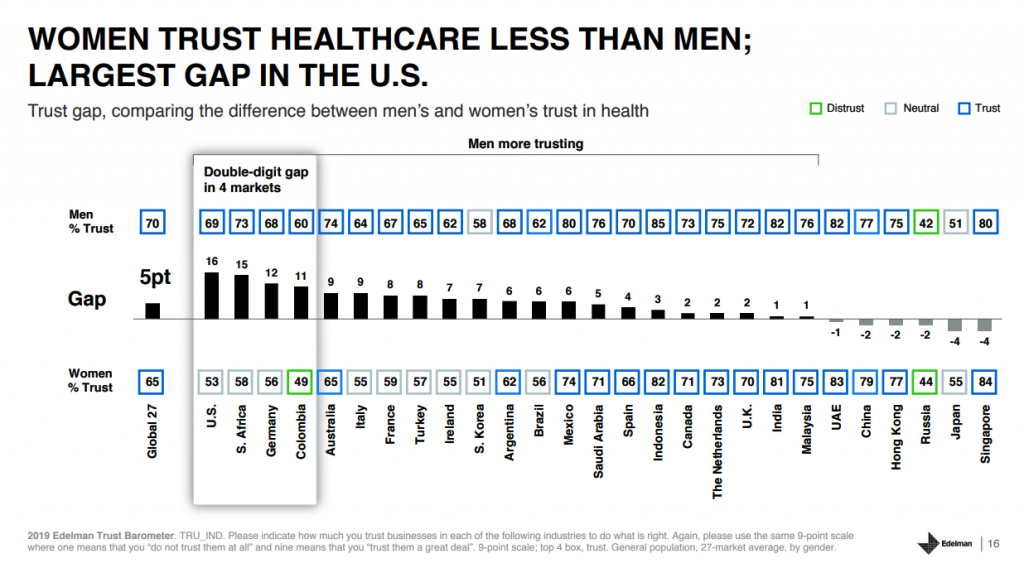
Fewer American women, too, trust the healthcare industry than men do.
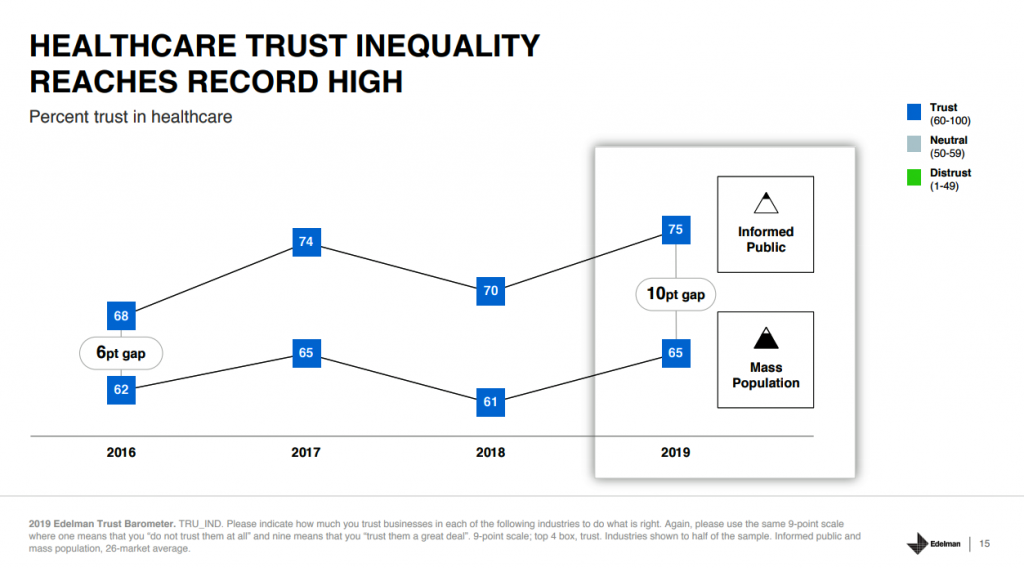 “This inequality of trust may be reflective of the mass population continuing to feel left behind as compared to others, even as they recognize the advances that are being made that could benefit them. Given tone and tenor of the day, and particularly among mass population, healthcare may continue to see increasing demands for change and regulation,” Susan Isenberg, Edelman’s head of healthcare, notes in her observations of the 2019 Edelman Trust Barometer.
“This inequality of trust may be reflective of the mass population continuing to feel left behind as compared to others, even as they recognize the advances that are being made that could benefit them. Given tone and tenor of the day, and particularly among mass population, healthcare may continue to see increasing demands for change and regulation,” Susan Isenberg, Edelman’s head of healthcare, notes in her observations of the 2019 Edelman Trust Barometer.
This week, Edelman released more granular healthcare insights from the annual omnibus survey that was published during the World Economic Forum in Davos in January. I analyzed those general results with health/care implications here in Health Populi.
In this study, the healthcare industry is comprised of five segments: hospitals and clinics; pharma; biotech (separate from pharma); consumer health (e.g., over-the-counter medicines); and, health insurance.
Trust in the overall healthcare industry grew by 4 percentage points on a global basis, with a net trust score of 67 points in the Edelman Trust index. This falls behind the top-trusted industry, tech, garnering 78 points, followed by manufacturing, education and automotive at 70, and retail at 69. Healthcare’s score is marginally greater than fashion, energy, consumer packaged goods, and financial services at the bottom at 57 points.
It’s important to note differences in trust across the five healthcare industry segments — and there are big differences. Pharmaceuticals garner the lowest score at 57, compared with biotech and life sciences at 64. While hospitals and clinics have the highest index across the five sectors, there was a decline in trust for providers — whereas the other four segments enjoyed trust increases.
What might account for this drop in trust for healthcare providers? My hypothesis would include the growing high-deductible world where patients facing high-cost hospital bills, sometimes surprise bills due to lack of transparency of costs and/or out-of-network “gotchas.” In addition, there is a growing risk of cybersecurity hacks of patients’ personal health information, with stories reaching local news media on a regular basis.
Compared with other countries, Americans’ trust in hospitals/clinics is on the lower end of the spectrum, just ahead of South Africa, Germany, Turkey, Colombia and Russia. The high index marks for hospitals were found in China at the top end (at 88), Indonesia, UAE, The Netherlands, and Malaysia.
The trust-gap between women and men is striking in the U.S. Not only do fewer women trust American healthcare, but that trust gap is the largest in the world across all countries Edelman polled, shown in the second graph.
 As we have noted for several years here on Health Populi, roughly equal proportions of Americans would trust digital companies and large retailers to help them manage personal health as trust health care providers.
As we have noted for several years here on Health Populi, roughly equal proportions of Americans would trust digital companies and large retailers to help them manage personal health as trust health care providers.
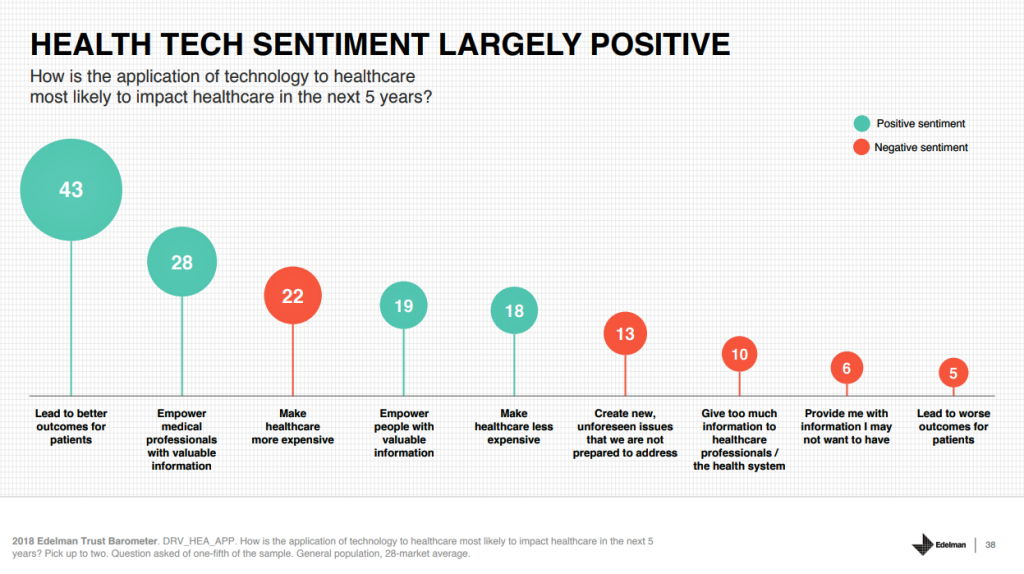
Edelman’s Trust Barometer measured consumers’ health tech sentiment, shown in the third graphic which captures peoples’ forecast on how tech will impact healthcare in the next five years. Leading to better outcomes, and empowering clinicians with useful information, could positively shape healthcare in the near term. However, tech could also make healthcare more expensive and create unforeseen issues we’re not prepared to address, consumers also expect.
Health consumers in America in the post Facebook/Cambridge Analytica era are much more attuned to privacy and cybersecurity risks of personal health data. Edelman identified three practices that would help U.S. health citizens in feeling more comfortable sharing their personal data:
- The company would place data in the most secure data protection system available
- The privacy of personal data would be guaranteed by the government, and
- The government or company or provider would guarantee that no one would ever link personal data back to “me.”
Ultimately, to earn and sustain trust with people, healthcare organizations — the five segments — should be transparent about the costs of products and services, provide balanced information about both benefits and side effects, and provide tools and support to help people manage their health.
Health Populi’s Hot Points: There is much to mine for health/care industry stakeholders in Edelman’s 2019 Trust poll at this particular moment-in-time for U.S. health consumers. The first layer concerns how trust between what Edelman segments as the “informed public” versus the mass population. There is a 10 percentage point gap between the informed public’s trust in U.S. healthcare compared with trust among the mass population.
Edelman defines the informed public as U.S. adults ages 25-64, college educated, in the top 25% of household income, who are avid, engaged consumers of media for business and public policy news.
By that definition, the informed public represents a higher socioeconomic stratum than the mass population, are more news-informed, and would likely be employed with access to employer-sponsored health insurance.
It’s no surprise, then, that trust among this U.S. population segment would run substantially higher than that among mainstream Americans.
Secondly, we see a significant gap in healthcare trust among U.S. women compared with men — the highest chasm in the world across all nations Edelman studied.
Susan Isenberg rightly pointed out in her analysis that women tend to be the “Chief Medical Officers” of their households.
I would expand that to be the “Chief Household Officers,” beyond medical and health/care issues. Women determine most health/care spending in their homes. At the same time, women have borne a “pink tax” for household goods and, indeed, healthcare prices, a topic I covered here in the Huffington Post a while ago in an essay I titled, “The Gender Disparity of Taxes: Toys, Tech and Tampons.”
 Cost continues to be top-of-mind for healthcare consumers, who largely blame pharma first in the Edelman research. This data point gives further impetus to prescription drug price hearings in Congress and various proposals promulgated on Capitol Hill to address the cost of medicines.
Cost continues to be top-of-mind for healthcare consumers, who largely blame pharma first in the Edelman research. This data point gives further impetus to prescription drug price hearings in Congress and various proposals promulgated on Capitol Hill to address the cost of medicines.
I write this as I received an announcement that Amazon has begun to more visibly market PillPack, the subscription mail service for prescription drugs in convenient medication-adherence packaging.
Amazon is also piloting selling health insurance in India. As health consumers in the U.S. continue to embrace new options for sourcing, consuming and paying for health care services, from “care” to supplies like prescription drugs and food-as-medicine, we can expect people to seek trusted channels for health engagement beyond the legacy system of hospitals, traditional health plans, and pharma.
The post Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical appeared first on HealthPopuli.com.
Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical posted first on http://dentistfortworth.blogspot.com
Tuesday 23 April 2019
Should we be spending more on pharmaceuticals?
Perhaps the answer is yes according to research from Frank Lichtenberg.
Every year, according to Lichtenberg’s research, drugs launched since 1982 are adding 150 million life-years to the lifespans of people in 22 countries that he analyzed. He calculated the average pharmaceutical expenditure per life-year saved at $2,837 — a bargain, he says.
“According to most health economists and policymakers, if you could extend someone’s life by a year for less than $3,000, that is highly cost effective,” says Lichtenberg, who gathered new data for these studies to cast a never-before seen view of the econometrics of prescription drugs. “People might be surprised by how cost-effective drugs appear to be in general.”
…Between 1982 and 2015, for example, the US saw the launch of 719 new drugs, the most of any country in the sample; Israel had about half as many launches. By looking at the resultant change in each country between mortality and disease, Lichtenberg calculated that the years of life lost before the age of 85 in 2013 would have been 2.16 times as high if no new drugs had been launched after 1981. For a subset of 22 countries with more full data, the number of life-years gained in 2013 from drugs launched after 1981 was 148.7 million.
For more details, see the Columbia University write-up and the original NBER working paper.
Should we be spending more on pharmaceuticals? posted first on http://dentistfortworth.blogspot.com
Monday 22 April 2019
The history of general practitioner contracting in the UK
A paper by McDermott et al. (2019) examines how primary care services are commissioned in the United Kingdom under the National Health Service (NHS). Interestingly, the study provides a nice overview of the history of GP contracting in the UK as well. An excerpt is below.
The current primary care system in England, whereby GPs [general practitioners] are contractors to the NHS, was born out of the decision made at the establishment of the NHS in 1947. This enabled GPs to remain independent to the NHS, minimising their opposition to the NHS. There was little planning for GP services from 1948 to 1990. GPs were contracted as individuals and payment were governed by the number of registered patients and by the services provided. GP contracts were administered by executive councils (1948–1972) whose membership included heavy representations of GPs themselves.
A unified system of administration was introduced in 1973 which integrated the planning and delivery of hospital services (administered by hospital boards), GP services (administered by executive councils) and personal health services (administered by local authorities such as maternity services, vaccination and ambulance services)…
The internal market was created in 1989 by the conservative government, introducing a split between the purchasers and providers of care, with a view to using competition between providers to achieve better ‘value for money’. Purchasers would ‘commission’ health services from providers by entering into contracts to deliver an agreed volume of services at a price. Purchasing would be more than simply contracting with and paying for providers to supply health services; providers would be made to compete for resources to encourage greater efficiency, responsiveness and innovation…
In spite of a rhetorical commitment to competition, payments of GP practices continued to be governed by a set of rules, with little local control over service development or provision. The notion of active commissioning started to gain prominence when the new labour government came to power in 1997. Responsibility for commissioning all types of services for a geographical population was given to newly established primary care trusts (PCTs), who were encouraged to start using a wider variety of contractual mechanisms to encourage new entrants into the primary care system… During the 2000s…contracts could be held by non-traditional service providers, including private companies, and they could be adjusted to specify a different range of services. PCTs were thus encouraged to actively shape the supply of services in their areas, introducing competition and actively procuring services to meet population needs.
Source:
- McDermott I, Checkland K, Moran V, Warwick-Giles L. Achieving integrated care through commissioning of primary care services in the English NHS: a qualitative analysis. BMJ open. 2019 Apr 1;9(4):e027622.
The history of general practitioner contracting in the UK posted first on http://dentistfortworth.blogspot.com
How to Prepare Your Child for the First Trip to the Dentist
How happy do you feel when you see your child completing milestones? The first step, the first word, and the first smile. These are all wonderful experiences that a parent will never forget.
We’re sure you felt a leap of joy when you saw your child had sprouted his or her first tooth, too. And that joy is natural because, at this stage, that will also mean your babe will soon be eating a more diverse diet, too.
After celebrating this event, it’s also time to think about another “first” for your child—his or her first visit to the dentist.
Starting dental visits at a young age can greatly increase the odds that your child will maintain good oral health and a sparkling white smile through life. But how do you get your child prepared for the chair? Are you concerned the experience will be intimidating?
Let’s jump in and see how you can quickly and simply get your child read!
When should a child visit the dentist for the first time?
In general, it’s recommended that children should have their first dental visits no more than six months after the appearance of their first tooth. Starting dental visits at such a young age can play an important role in the oral health of your child later in life.
To begin with, baby teeth may not be permanent, but they can cause issues in speaking and chewing if they are not healthy.
What’s more, tooth decay can occur as soon as your child’s first tooth pops, and having tooth decay on baby teeth can further increase the risk of having tooth decay in permanent teeth.
And, perhaps the most important reason yet, starting dental visits at a young age can help build the habit of proper dental care and grow familiarity with dental procedures so that these don’t cause anxiety in the future. Building these routines at such a young age can greatly increase the odds that your kids will keep those healthy habits throughout life.
How to prepare your child for the first dentist visit
The first dental visit for your child can end up being frightening—for your child and for you—if he or she isn’t prepared. But these simple tips can help get everyone on board for a stress-free dental visit!
Tip #1: Practice at home
It’s very important for your child to get accustomed to having hands and fingers in and around the mouth before visiting the dentist for the first time.
What’s a hygienic and safe way to go about this? Try Running a soft, wet washcloth or a toothbrush specially designed for infants over the gums and teeth. This both cleans your child’s teeth and gets him or her accustomed to having hands and dental tools in the mouth. Songs and games can reinforce this routine.
Tip #2: Begin teaching your child about teeth
Children love exploring and learning new things! Teaching your child about his or her teeth and mouth will not just be a way to get interested in oral health, but will also make the first dental appointment easier.
Since we’re talking about starting these practices at a very young age, simply teaching your child to identify where everything is in its mouth is enough for now. Songs, games, giving names to teeth can help here as well!
Tip #3: Explain what to expect at the dentist’s office to your child
Your child’s first dental visit will not involve any pain. The dentist will devote time to gently examine your child’s teeth—and maybe clean them if necessary. At Dr. Ku’s office, we make the visit a fun experience in order to create a positive association with dental visits.
In addition, games like using a stuffed animal as a “dentist” in play or teaching your child how to be the dentist by allowing him or her to “examine” your teeth will definitely be fun and help your child become familiar with the process.
Your child’s first dental appointment can very easily become a fun experience if you practice beforehand with fun and games! Follow the list above, and you will experience a tear-free first visit.
The post How to Prepare Your Child for the First Trip to the Dentist appeared first on Fort Worth Dentist | 7th Street District | H. Peter Ku, D.D.S. PA.
How to Prepare Your Child for the First Trip to the Dentist posted first on http://dentistfortworth.blogspot.com
Sunday 21 April 2019
Do consumers make rational choices for their Part D Plan?
To answer this question, one can examine how individuals choose health plans based on premiums, expected out of pocket cost, plan quality, and other factors. A paper by Abaluck and Gruber (2011) use data from 2006 and find that up to 70% of seniors appear to choose plans that are not optimal. Do these conclusions hold with more recent data? And are there improved methods for answering this question.
One question is how does one treat the error term in these regressions. In a standard random utility model, the error term captures heterogeneous tastes for unobserved product attributes. People are not perfectly rational, however, and thus the error term could also capture optimization error, genuine randomness in decision making, or other types of confusion.
To answer this question and examine whether PDP plan choice has improved in more recent data, a working paper by Keane et al. (2019) use a finite mixture of mixed logit model or MM-MNL model. Their basic approach uses the following model:
U_ij = (Pj)α+[E(oop)ij]β1 + (σ^2_ij)β2 + (cj)β3 + (Qj)β4 + e_ij
In this equation, P is the premiums for plan j, E(oop) is the expected out of pocket costs, σ^2_ij is the variance in out of pocket costs, cj, is a vector of financial characteristics of plan j that affect OOP, and Qij is a vector of plan quality measures, which in this study includes both star ratings and indicator variables for plan “brand”.
The authors initially conceive of 2 latent classes of individuals. The rational, risk neutral individual would be indifferent to premiums and out of pocket costs (assuming the impact from discounting is small given the 1 year time horizon covered by Part D Plans) and thus α = β1. Also rational individuals should be indifferent among different financial characteristics (cj) that lead to the same E(oop) and σ^2_ij and thus β3=0. In short, we can divide the world into rational individuals where utility is defined as:
U_ij = [Pj + E(oop)ij]β1 + (σ^2_ij)β2 + (Qj)β4 + e_ij
with probability p and with probability 1-p individuals are not rational and have utility as described in the first equation. In short, conditional on a person’s latent type (i.e., rational vs. not) and his/her preference parameters, we have a simple multinomial logit model.
The authors also extend this model by: (i) considering more than two types where the “rational” type is defined as above, and the data is used to determine the other types and (ii) the authors let individual characteristics (e.g., age, presence of Alzheimers’ disease, depression) affect individual decision-making ability.
The authors highlight the benefit of their model, saying:
Given estimates of the decision utilities of the confused type, as well as the distribution of their parameter vector ), we can learn how their behavior is sub-optimal. Do many consumers…place excessive weight on premiums vs. OOP costs? Or are these excesses statistically significant but quantitatively small? Are there particular “irrelevant” financial attributes of insurance plans that consumers tend to overweigh in making decisions?
The authors then use PDP administrative data from non-low income subsidy individuals as well as data from the Medicare Current Beneficiary Survey to test this approach.
The authors have a number of interesting findings. First, individuals place more weight on premium reduction than reducing future out-of-pocket cost. Second, a plan’s brand plans an important part in plan choice for some consumers. In general, fewer than one-in-ten consumers are perfectly rational from an economist’s defminition..
…we find that 9.8% of consumers are classified as the “rational” type, while 11.4% place excess weight on low premiums, and 78% place value on plan characteristics that are irrelevant once one conditions on the distribution of plan costs…As expected, people with dementia and depression are more likely to be “irrational.” And the bulk of the econometric error term is attributed to optimization error
A more important question may be, does this matter? If people are choosing incorrectly, are these error costing them $5 per year or thousands of dollars? The authors perform a welfare analysis to see how welfare would improve if people picked a more optimal plan.
…we find welfare losses to be modest except in a small subset of cases (e.g., people with dementia and depression face a high variance of OOP costs, suggesting they are not well insured). In contrast to traditional choice models, in our framework consumer welfare can be enhanced by eliminating “bad” options from the choice set. But as in Ketcham et al. (2019) we find that such policies lead at best to trivial welfare improvements. This occurs for two reasons: (i) Part D premiums are heavily subsidized, so even a “bad” plan is better than no plan, and (ii) given consumer heterogeneity, very few plans are “bad” for everyone.
Do consumers make rational choices for their Part D Plan? posted first on http://dentistfortworth.blogspot.com
Thursday 18 April 2019
Links
- Health Utility Book (HUB)
- Can doctors talk teenagers out of risky drinking?
- Impact of physician disclosures on patient trust.
- Quadratic voting in practice.
- Why doctors don’t like email.
Links posted first on http://dentistfortworth.blogspot.com
Telehealth In 2030 – Notes From the Future At #ATA19 with Safavi, Holt, Bathina and Swafford

 Kim Swafford of Providence St Joe’s knows a lot about telehealth “today” because her organization is on the forefront of leveraging digital and virtual health modes. Providence St. Joe’s deploys telehealth in eight states. She asserts that leveraging AI and machine learning for low acuity issues can automate as much as 80% of care, for both physical and behavioral/mental health.
Kim Swafford of Providence St Joe’s knows a lot about telehealth “today” because her organization is on the forefront of leveraging digital and virtual health modes. Providence St. Joe’s deploys telehealth in eight states. She asserts that leveraging AI and machine learning for low acuity issues can automate as much as 80% of care, for both physical and behavioral/mental health.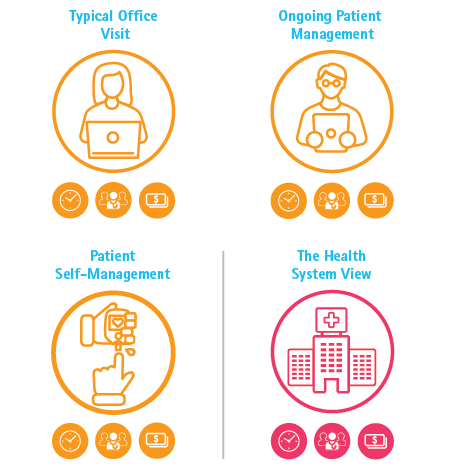 Health Populi’s Hot Points: In full disclosure, I worked with Kaveh and the Accenture team on a recent study modeling the economic value of shifting a portion of ambulatory care visits to virtual care settings. The report’s title summarized what we calculated: Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare. We modeled three scenarios: a typical primary care office visit, ongoing patient management dealing with a chronic condition, and patient self-management at home. Our scenarios combined virtual health and traditional in-person patient care to reflect a hybrid model of care, reflecting how life really works in an omni-channel world for healthcare and other daily life-flows. By saving even five minutes’ time per patient, our model calculated that a health system could conserve 320 primary care providers (PCPs) and save about $63 million for these three use cases taken together.
Health Populi’s Hot Points: In full disclosure, I worked with Kaveh and the Accenture team on a recent study modeling the economic value of shifting a portion of ambulatory care visits to virtual care settings. The report’s title summarized what we calculated: Virtual Health: The Untapped Opportunity to Get the Most out of Healthcare. We modeled three scenarios: a typical primary care office visit, ongoing patient management dealing with a chronic condition, and patient self-management at home. Our scenarios combined virtual health and traditional in-person patient care to reflect a hybrid model of care, reflecting how life really works in an omni-channel world for healthcare and other daily life-flows. By saving even five minutes’ time per patient, our model calculated that a health system could conserve 320 primary care providers (PCPs) and save about $63 million for these three use cases taken together.The post Telehealth In 2030 – Notes From the Future At #ATA19 with Safavi, Holt, Bathina and Swafford appeared first on HealthPopuli.com.
Telehealth In 2030 – Notes From the Future At #ATA19 with Safavi, Holt, Bathina and Swafford posted first on http://dentistfortworth.blogspot.com
Instrumental variables: Can I use patient level IVs to correct for endogeneity in patient characteristics?
Does a treatment improve patient health? Does a policy intervention improve quality of life? Does more education increase income? These are fundamental questions that are difficult to answer with standard observational approaches. The reason? Selection bias.
Patients who are sick take medicine; patients who are sicker may take more medicine. Thus, one could observe that patients who take highly effective medicine have worse outcomes not because of any causal relationship but because sick people are the ones taking medicine.
One way to account for selection bias is to use instrumental variables. An instrument must satisfy 3 key conditions:
- It must be correlated with the potentially endogenous treatment variable;
- It must have no direct effect on the outcome (other than through its impact on the probability of treatment); and
- It must be independent of the unmeasured confounders of the treatment–outcome relationship after conditioning on the measured confounders (See Garabedian et al. 2014 for an explanation)
What if a researcher wants to know if certain physician or hospital characteristics are associated with better patient outcomes. In standard analyses, if unobservable better quality physicians prefer to live in rich areas where patients have unobservably better baseline health and these physician characteristics are correlated with observed characteristics, it could be the case that researchers misattribute a causal effect to a specific physician attribute.
Can patient-level variables serve as an instrument for provider characteristics? According to a paper by Konetzka et al. (2019), at first, the approach seems promising.
Take the example of estimating the effect of for‐profit status of a hospital on patient outcomes. Patients treated at for‐profit hospitals may be different in unmeasured ways from patients treated at other hospitals—in preferences for preventive care, level of social support, or health status. To solve this problem, an instrument Wi can be used. A logical choice may be the differential distance instrument, using the additional distance a patient would have to travel to reach a for‐profit hospital versus the nearest hospital. The use of this instrument could result in groups of patients that are balanced on observed and unobserved characteristics, minimizing confounding by patient selection
This approach may be valid of physician characteristics are not selected (e.g., male gender). However, some physicians/organizations may choose their characteristics. Physicians may choose their specialty; hospitals may deicde strategically whether to be a for-profit or non-profit entity. In the case of measuring the effect of being a for-profit hospital, researchers would need an instrument that “exogenously pseudo‐randomizes hospitals to be for‐profit—say, an instrument based on what competitor hospitals in the market are doing, or a change in laws about for‐profit status”.
Using both instruments may be valid, but using only the patient-level instrument to control for provider level selection bias is problematic.
It is a mistake, however, to use a patient‐level instrument Wi to attempt to solve the endogeneity of an organization‐ level treatment variable or to imply that it does. If the goal of the analysis is to estimate a causal effect of for‐profit status, an erroneous approach might be to use patient‐level differential distance as an IV. Although this would likely result in treatment and comparison groups balanced on patient‐level characteristics, it does nothing to solve the critical provider selection issue.
The authors claim that the Joyce et al. (2018) paper does the best job of addressing the provider selection issue. While they also use a patient-level instrument, they also conducted a series of robustness checks using a dose–response strategy based on the percent of patients in a dementia Special Care Unit and comparisons to patients without dementia in order to isolate the causal effect of Special Care Units from unmeasured hospital quality.
Source:
- Konetzka RT, Yang F, Werner RM. Use of instrumental variables for endogenous treatment at the provider level. Health economics. 2019 Jan 22.
Instrumental variables: Can I use patient level IVs to correct for endogeneity in patient characteristics? posted first on http://dentistfortworth.blogspot.com

