The supply side of digital health tools and tech is growing at a hockey-stick pace. There are mobile apps and remote health monitors, digital therapeutics and wearable tech from head-to-toe. Today in America, electronic health records (EHRs) are implemented in most physician offices and virtually all hospitals. Chapter 5 of my book, HealthConsuming: From Health Consumer to Health Citizen, details the promise of digital health: wearable, shareable and virtual.
 Today, we can also call on Alexa to remind us to take medications, play nostalgic music when we are lonely, check our physical activity status with Fitbit, and query WebMD about a symptom. Just last month, Amazon announced HIPAA-compliant privacy bundled into Alexa skills with Atrium Health, Boston Children’s Hospital, CIGNA, ExpressScripts, Livongo, and Swedish Health Connect.
Today, we can also call on Alexa to remind us to take medications, play nostalgic music when we are lonely, check our physical activity status with Fitbit, and query WebMD about a symptom. Just last month, Amazon announced HIPAA-compliant privacy bundled into Alexa skills with Atrium Health, Boston Children’s Hospital, CIGNA, ExpressScripts, Livongo, and Swedish Health Connect.
Broadband connectivity, cloud computing, data analytics and well-conceived artificial intelligence (AI) enable the use of data generated from digital health tools to benefit our health. Increasingly, as connectivity gets to each of us wherever we live, work, play, and learn, and sensors shrink and lower in cost, we can do more self-care at home and in lower-cost venues to help bend that stubborn medical cost curve. This is a health economist’s Holy Grail, and my vision for the home-as-health-hub which is my end-image in HealthConsuming.
As I walk the miles of aisles at the annual CES, I track ten technology categories that can support this paradigm, covering more mature digital health tech like WiFi weight scales and personal emergency response systems to the growing Internet of Things ecosystem for smart and connected homes and cars, an emerging third space for health that Honda, Mercedes, Toyota, et. al., are concepting, which I wrote about back in 2007 focusing on Toyota’s wellness car concept.
Promising, promising.
With every one of these digital health encounters, from Alexa to Zipongo, a bit of data is created. It’s personal stuff, and it’s a tiny little bit about “you.”
All that digital dust can be collected, mashed up and built into a personal profile for your benefit, or for other reasons. The graphic is based on work done by Juhan Sonin of GoInvo, a group that does brilliant work on health data design that’s vigilantly people-focused. GoInvo has been working for a long time on how to communicate health and healthcare data in enchanting ways.
Juhan and another person first shaped my views converging the promise of digital health data through enchanting design, and the perils of Big Data algorithms. Juhan for the former lightbulb moment; and for the latter, Fred Trotter. I interviewed Fred for research I was conducted on behalf of the California HealthCare Foundation (CHCF) in 2014.
For CHCF that year, I wrote Here’s Looking at You: How Personal Health Information is Being Tracked and Used, I took cues from a 60 Minutes‘ profile of third-party data brokers and Latanya Sweeney’s groundbreaking research at the Harvard Privacy Lab. Latanya found that just a few data points — which fell out of HIPAA-privacy protected flows — could re-identify a person with, say, HIV positive status, a mental health DSM-code, or degenerative disease.
Five years later, patients still share their personal health information on Facebook groups, with the promise of crowdsourcing cures, accessing support and advice, and finding community.
As a WEGO Health poll of patient activists found in April 2019, patients continue to share this very intimate data, even in the wake of the Facebook/Cambridge Analytica story, growing cybersecurity breaches of medical data, and a challenging environment for trust and “fake news” for health care.
In researching the thorny privacy issues for HealthConsuming,. I learned the phrase “a concerned embrace of technology” from Deloitte’s 2017 survey of U.S. mobile consumers. Deloitte found that 80% of consumers believed that companies were using their personal data and that their data wsa being shaerd with third parties. But people were williong to share “some” online data (like name or email address), less willing to share health metrics using a phone or wearable device — only 7% of people willing to do that in 2017 based on this poll.
So “concerned embrace” for health means that trust is the enabling bridge between digital health connections and peoples’ willingness to share data — underpinned by stronger privacy protections and true data ownership for each person. Through that ownership and control, people could monetize their own data and treat it as the personal asset it truly is.
This is the plotline between HealthConsuming‘s Chapter 5 on the promise of “Digital Health: Wearable, Shareable, Virtual” and Chapter 6 on “Privacy and Health Data In-Security.”
Tomorrow will be my fifth and final post in this week’s series outlining HeatlhConsuming: From Health Consumer to Health Citizen, focusing on the last two words in the title. Can and will Americans take on the role of health citizens, with health care access as a civil right and full privacy protections, coupled with the responsibilities for self-care and health engagement, and the civic responsibility to vote and engage in civil discourse? We’ll round out this journey in tomorrow’s Health Populi.
That’s the argument for health citizenship, our topic for tomorrow’s #5 of five posts plotlining HealthConsuming: From Health Consumer to Health Citizen, all this week in the Health Populi blog.
The post The Promise of Digital Health and the Privacy Perils – HealthConsuming Explains, Part 4 appeared first on HealthPopuli.com.
The Promise of Digital Health and the Privacy Perils – HealthConsuming Explains, Part 4 posted first on http://dentistfortworth.blogspot.com
 Today, the Brookings Institution convened a meeting on
Today, the Brookings Institution convened a meeting on 
 As patients now assume the role of health consumer, they rationally expect retail-level experiences with greater first-dollar payment for health insurance, health care services and medical products like prescription drugs.
As patients now assume the role of health consumer, they rationally expect retail-level experiences with greater first-dollar payment for health insurance, health care services and medical products like prescription drugs. People trust Amazon for daily retail experiences. The bar chart from research by Market Strategies shows that a plurality of consumers also trusts Amazon to try on for healthcare products and services. The company has been multi-tasking a broad range of tactics throughout the health care ecosystem. Every publicly traded market segment Amazon has touched has had moments of shattering stock prices.
People trust Amazon for daily retail experiences. The bar chart from research by Market Strategies shows that a plurality of consumers also trusts Amazon to try on for healthcare products and services. The company has been multi-tasking a broad range of tactics throughout the health care ecosystem. Every publicly traded market segment Amazon has touched has had moments of shattering stock prices. Jim Cramer of CNBC’s Mad Money has been studying up on digital health, recently recommending that Apple buy Epic, the health IT behemoth. (See more on that recommendation, and subsequent social media frenzy,
Jim Cramer of CNBC’s Mad Money has been studying up on digital health, recently recommending that Apple buy Epic, the health IT behemoth. (See more on that recommendation, and subsequent social media frenzy, 
 First, let’s explore the scenario-reality of the patient-as-payor, now consumer. This is a contentious issue, debated from my admired economist-guru Paul Krugman in the New York Times
First, let’s explore the scenario-reality of the patient-as-payor, now consumer. This is a contentious issue, debated from my admired economist-guru Paul Krugman in the New York Times 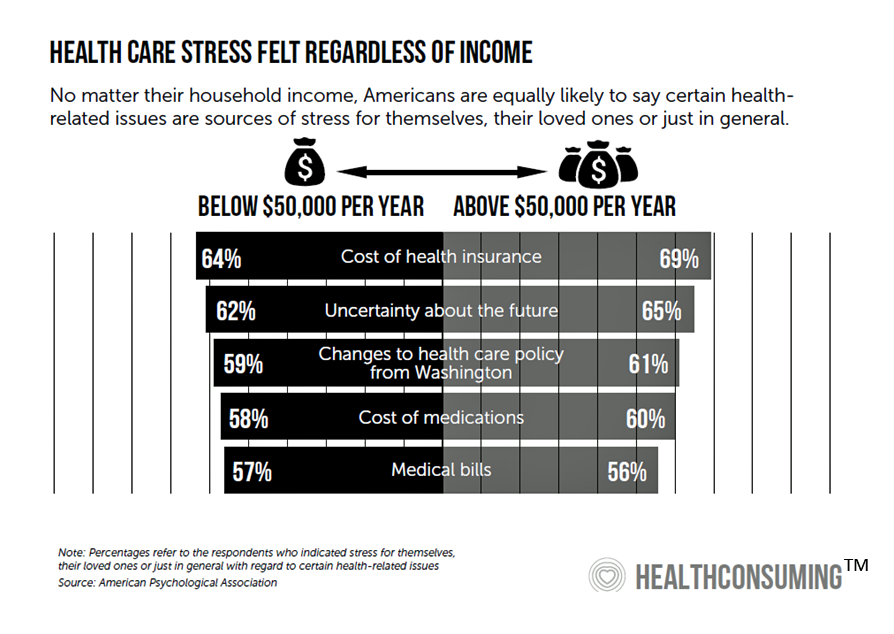 Health care costs stress out people at all income levels in the U.S.,
Health care costs stress out people at all income levels in the U.S.,