Sunday 31 March 2019
Friday 29 March 2019
Most Americans Blame Drug Companies, Insurers, and Hospitals for High Health Care Costs
There’s little agreement between Democrats and Republicans on a plethora of issues in American public life. But one issue that brings U.S. citizens together is agreement that the cost of health care is too high in the country, and that pharma, health plans, and providers are to blame.
 Welcome to health politics in America as of March 2019, according to The Public and High U.S. Health Care Costs, a poll conducted by POLITICO and the Harvard T.H. Chan School of Public Health.
Welcome to health politics in America as of March 2019, according to The Public and High U.S. Health Care Costs, a poll conducted by POLITICO and the Harvard T.H. Chan School of Public Health.
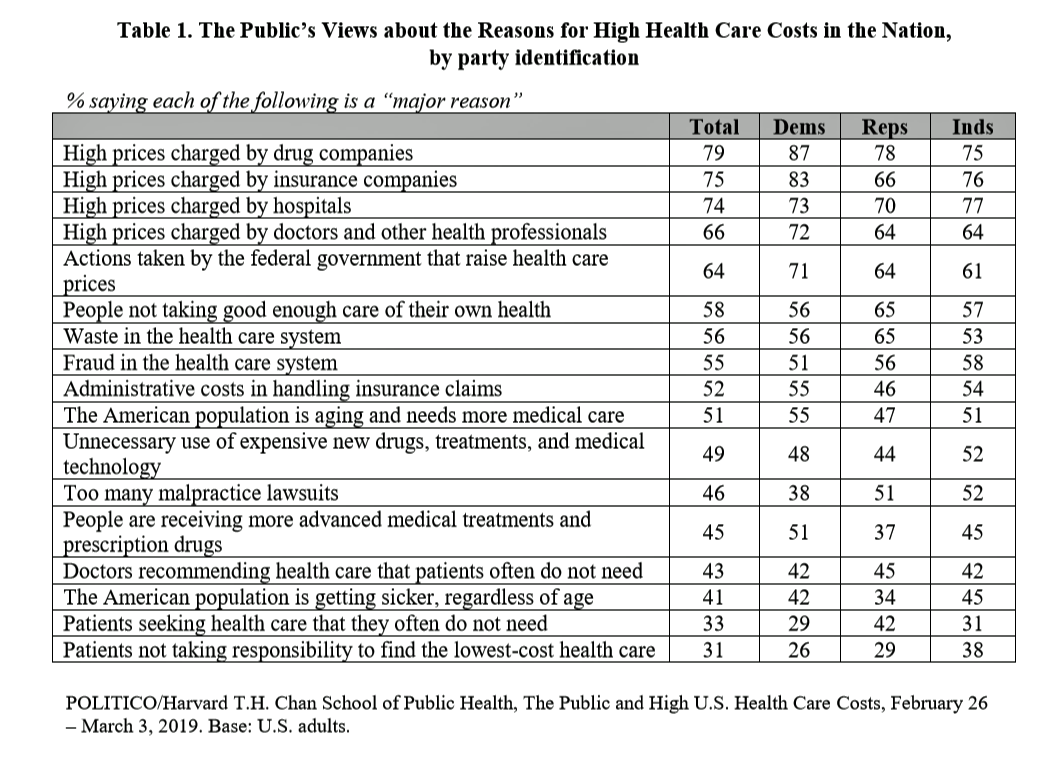
The first chart illustrates the common ground shared by Americans by party affiliation, with vast majorities across parties playing the blame game on healthcare industry groups.
Note that 58% overall believe another cost driver is people not taking good enough care of their own health, with 58% of Democrats, 65% of Republicans, and 57% of Independence blaming fellow citizens for lack of self-care. A similar percentage overall blames waste, fraud and administrative costs in the system for high health care spending in America.
Patients over-using care and not shopping around on the basis of price garner the lowest percentages of blame, with about 1 in 3 people ascribing blame to these factors.
One of the larger delta/differences on this list between Democrats and Republicans relates to people receiving more advanced medical treatments and prescription drugs: 51% of Democrats blame high costs on newer treatments, while only 37% of Republicans do so.
How can the U.S. reduce the high cost of health care? The most-agreed strategy would be to advance prevention of future disease and to ensure that people live healthier lives, cited by 84% of Americans, and fully 8 of 10 people across political party.
After this strategy, few solutions have this level of agreement across party divides. Most Republicans (74%) favor fostering greater competition between health care professionals and hospitals; 73% of Democrats point to the government capping prices on hospital and provider charges, allowing people 50-64 to buy into Medicare, and changing the health system so that most people have Medicare with little to no private insurance.
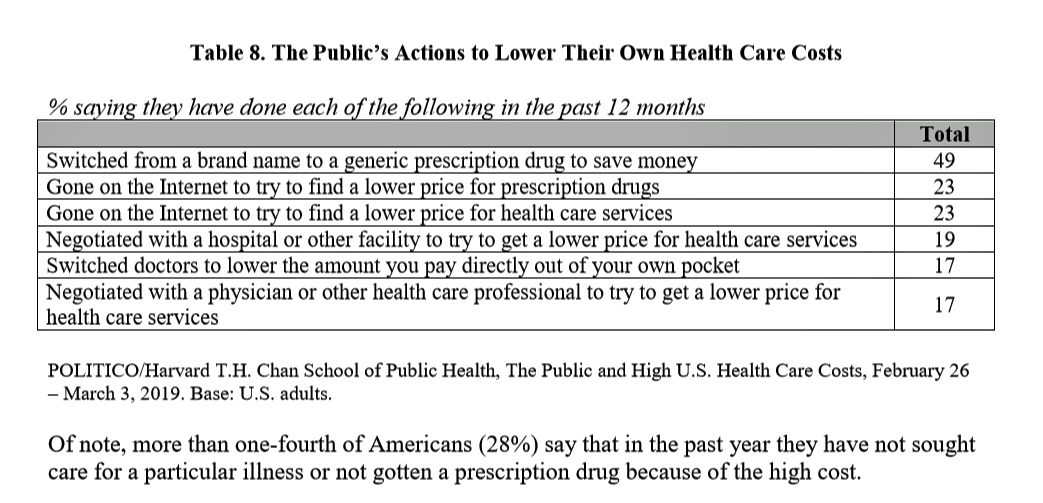
The most prevalent action individuals have taken to lower their own health care costs was to switch from a brand name to a generic prescription drug, done by 49% of Americans polled. Well below this cost-saving tactic were searching the Internet for lower prices for medicines, searching on the Internet to lower prices on health care services, negotiating with hospitals for lower prices, switching doctors to lower out of pocket costs, and negotiating with physicians for lower prices on services. The second chart details these health consumer strategies.
One in four U.S. consumers (28%) have not sought health care or filled a prescription drug due to the high cost — a cost-saving tactic done by 32% of Democrats, 24% of Republicans, and 25% of Independents.
Health Populi’s Hot Points: The broad consensus in America is that health care costs are too high, an opinion shared across political parties. And, most people in the U.S. told POLITICO and the Harvard team that prevention and health promotion embody the most important strategy for lowering health care costs in the nation. Competition and setting cost-limits were also majority-shared tactics across party affiliations.
 As for leveraging Medicare to cover more Americans as a cost-lowering strategy, health citizens are at-odds. Roughly one-half of people overall are concerned that Medicare will run out of money in the next decade. Americans are also split by party whether the Federal government versus State governments would be more effective at setting those health care prices.
As for leveraging Medicare to cover more Americans as a cost-lowering strategy, health citizens are at-odds. Roughly one-half of people overall are concerned that Medicare will run out of money in the next decade. Americans are also split by party whether the Federal government versus State governments would be more effective at setting those health care prices.
The researchers conclude that whichever party “dominates” the future leadership in the executive and legislative branches will determine the eventual approach to cost containment — Democrats would tend to seek greater government intervention, whereas Republicans would look for private insurance and competitive market forces.
The one major agreement is that prescription drug costs are too high, and generics are beloved by American health consumers looking for pills at a price.
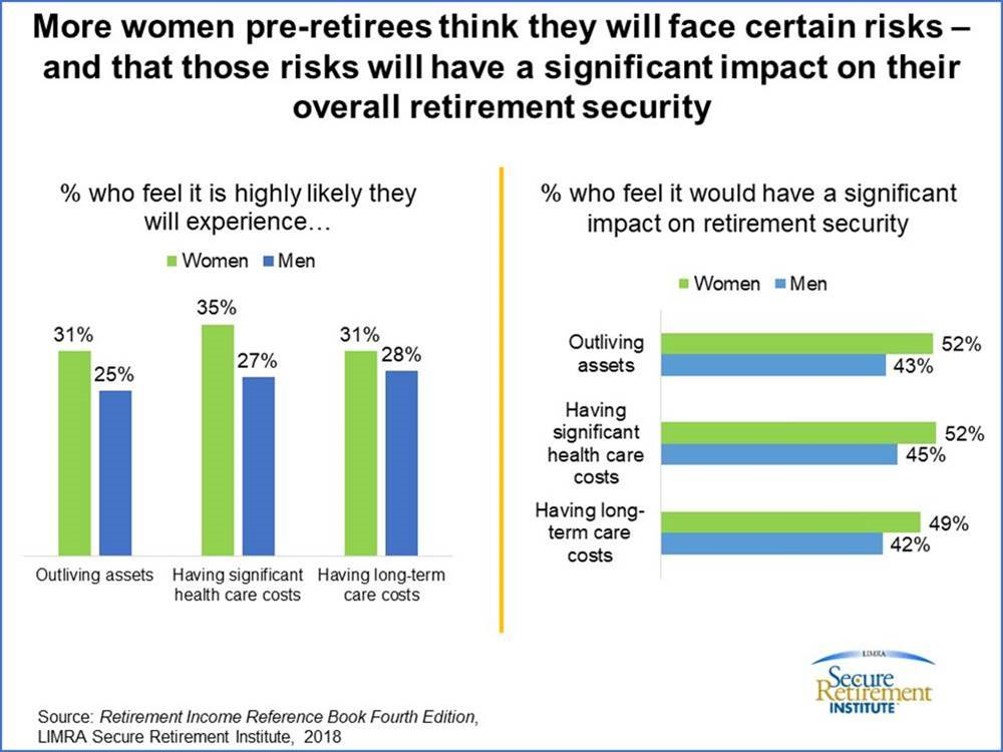
It’s certain that health care will dominate discussions between “now” and November 7, 2020, when health care will certainly drive people — and women, especially driven by medical cost concerns — to the polls. Why do I say this? The third chart informs my forecast, illustrating that women in pre-retirement are more concerned about health care and long-term care costs more so than men are. LIMRA wrote up this analysis in honor of National Women’s History Month as it draws to a close this month of March 2019.
I predict that the history of the 2020 Presidential election in the U.S. will drive a plurality of cost-and-coverage concerned women to the polls as health care voters.
The post Most Americans Blame Drug Companies, Insurers, and Hospitals for High Health Care Costs appeared first on HealthPopuli.com.
Most Americans Blame Drug Companies, Insurers, and Hospitals for High Health Care Costs posted first on http://dentistfortworth.blogspot.com
Friday Links
- Hospitals jump into telehealth.
- The cost of dementia.
- Are certificate of need (CON) laws needed?
- Myth of FFS and overprovision?
- Opening Day content: Born a Brewer and ‘Not today’
Friday Links posted first on http://dentistfortworth.blogspot.com
Thursday 28 March 2019
Our Mobile Health Data: Shared, Identifiable, and Privacy-Deprived
 As more mobile app users — consumers, patients, and caregivers — use these handy digital health tools, much of the data we share can be re-identified and monetized by third parties well beyond those we believe we’re sharing with.
As more mobile app users — consumers, patients, and caregivers — use these handy digital health tools, much of the data we share can be re-identified and monetized by third parties well beyond those we believe we’re sharing with.
This compromised health data privacy scenario comes out of research published this month in the BMJ, Data sharing practices of medicines related apps and the mobile ecosystem: traffic, content, and network analysis.
The researchers, faculty from the University of Toronto (Canada) and the University of Sydney (Australia), come from nursing, pharmacy, and computer science expertise — a sound combination of disciplines to ask the question, “how are consumer data shared by top rated medicines related mobile apps,” and to assess the privacy risks to app users. The authors look through both clinician and consumer lenses.
The research identified top-ranked health-related apps for Android mobile platforms available in Australia, Canada, the United Kingdom, and the U.S. The analysis started with 821 apps found through a crawling program and expert sources, and narrowed that app universe down to 24 unique apps for the analysis: 10 targeting health professionals, 11 focused on consumers, and 3 targeting both user-types.
The researchers then looked into the data transmitted to third parties among these apps, including the type of consumer data, volume of those transmissions, and the identities of the third parties with whom consumer data were shared.
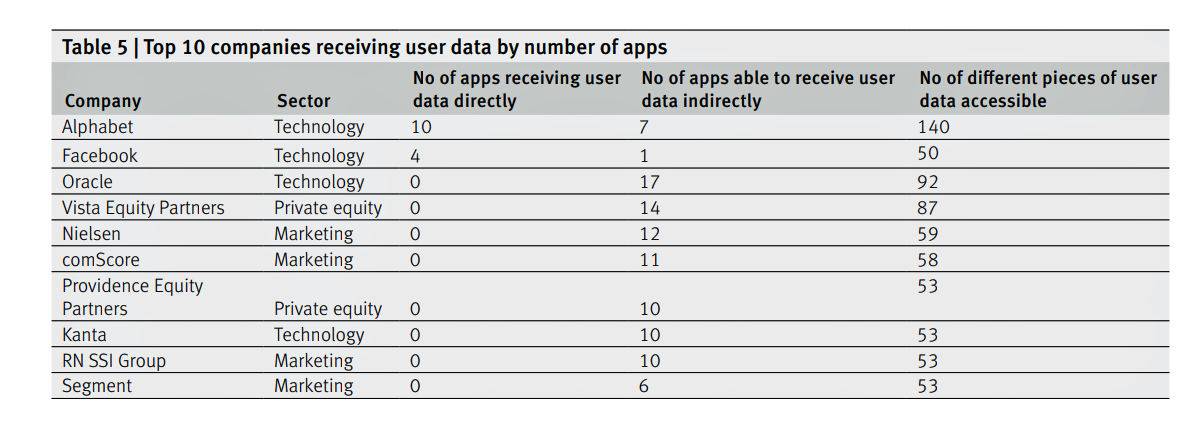
The first chart summarizes the top ten companies that received user data by the number of apps and pieces of user data. By far, the most active third party receiver was Alphabet/Google. Other companies trailed behind Google including Facebook, Oracle, Vista Equity Partners, Nielsen, and comScore.
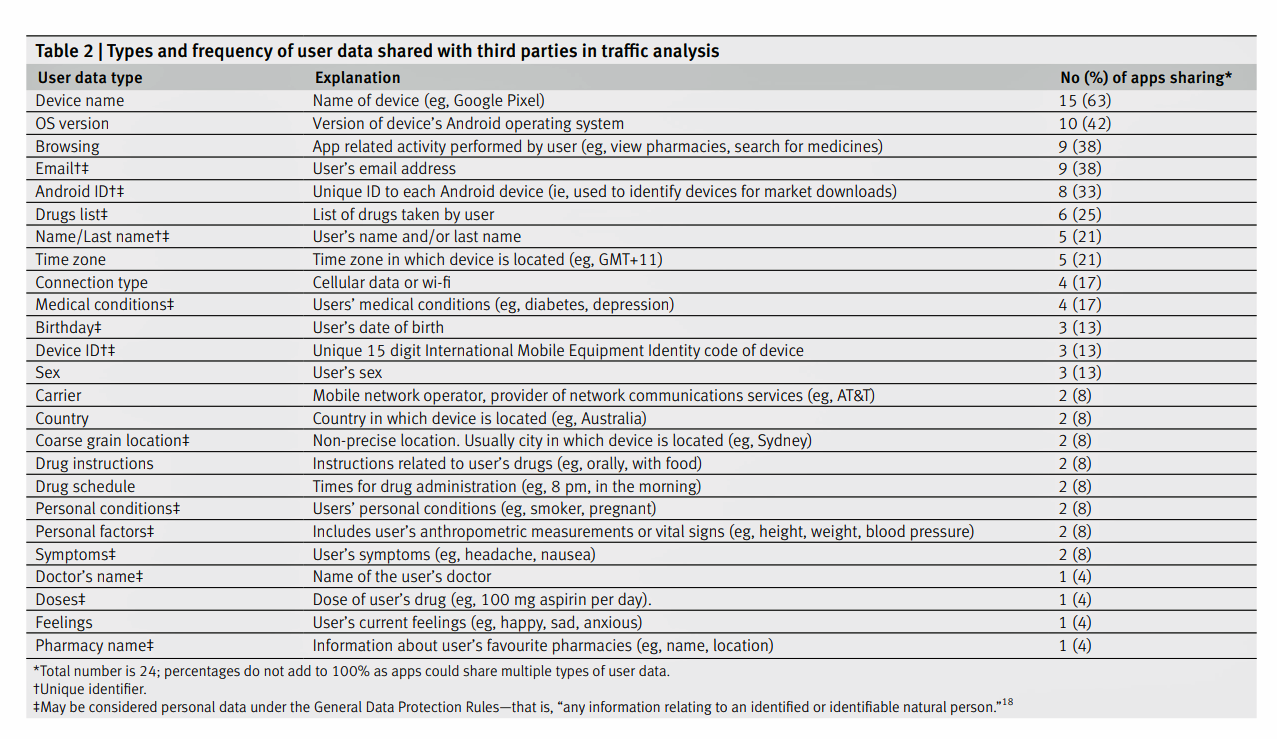
The second chart inventories the types and frequency of user data shared with third parties. The most common data types were device names, version of the operating system used, browsing history (e.g., pharmacies, prescription drugs), email addresses, and drug lists. User names were identified by one in five apps studied.
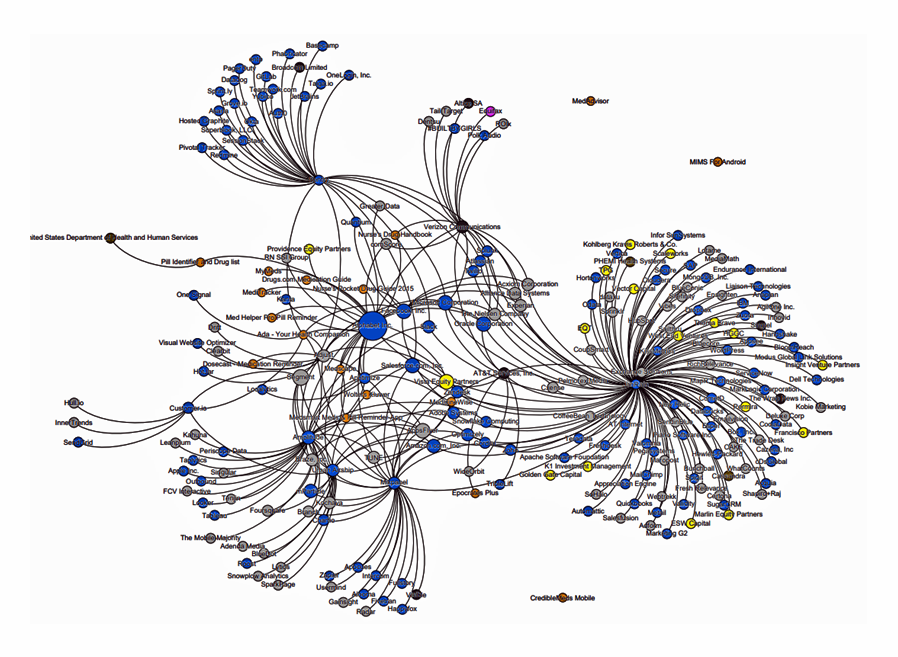 Beyond this third-party data analysis, the research identified fourth-party sharing in the mobile app ecosystem. Companies in the fourth party network receive consumer data for behavior analytics and advertising, among other applications, the article notes. The third graphic represents the fourth party data network of 237 entities — 17 app families, 18 third parties, and 216 fourth parties. The blue dots are typically software and technology companies (about 55% of the entities); the grey dots are digital advertising companies. Only three entities were related to healthcare (the brown dots).
Beyond this third-party data analysis, the research identified fourth-party sharing in the mobile app ecosystem. Companies in the fourth party network receive consumer data for behavior analytics and advertising, among other applications, the article notes. The third graphic represents the fourth party data network of 237 entities — 17 app families, 18 third parties, and 216 fourth parties. The blue dots are typically software and technology companies (about 55% of the entities); the grey dots are digital advertising companies. Only three entities were related to healthcare (the brown dots).
The prevalence of Google in this ecosystem is a key finding from the study. The authors call out that Alphabet, the parent company of Google, owns the third parties Crashlytics, Google Analytics, and AdMob By Google which were all in the ecosystem studied. In the company’s privacy policy Google reports data sharing partnerships with Nielsen, comScore, Kanta and RN SSI Group.
Beyond Google (Alphabet), the authors identify Facebook and Verizon Communications as “having received monopoly positions within the mobile ecosystem.”
The bottom-line conclusion: the collection of app users’ data is a business, but the lack of transparency and less-than-tenacious approach to securing users’ consent doesn’t benefit the consumer, the authors assert. They believe that users can be easily identified.
“Currently, within the ‘big data’ industry, users do not own or control their personal data,” the researchers conclude. “Regulators should focus on full transparency, requiring sharing as opposed to privacy policies…privacy will become an important social determinant of health.”
Health Populi’s Hot Points: I wrote Here’s Looking at You on behalf of the California Healthcare Foundation (CHCF) in July 2014, highlighting how third parties could access and mash-up data generated through digital tools — both consumer apps and health-focused ones, along with retail receipts and social network check-in’s.
The BMJ study is a welcome update to my work, especially as more consumers download and use mobile apps in daily life-flow, for managing both everyday life and, increasingly, to support their own and loved ones’ health. Consider the growing Internet of Things for health/care, connected car concepts baked with wellness, and the advances in voice tech that Alexa and her cousins from Google and Samsung are making to support our health at home and in that automobile. All of these new-new “things” are connected devices, generating personal data that can be scraped for our health profiles.
While California will implement a broad consumer-protective privacy law on January 1, 2020, the remainder of the U.S. remains covered by a patchwork quilt of laws that done comprehensively cover American health citizens. Congress is, currently, wrestling with creating an updated privacy law after more than a decade of Americans’ ubiquitous smartphone and social network adoption. Europe’s GDPR is widely recognized as the gold standard for privacy law. Will Americans benefit from a U.S.-style GDPR? Our digital life- and health-styles require that level of personal data ownership, control, and stewardship.
The post Our Mobile Health Data: Shared, Identifiable, and Privacy-Deprived appeared first on HealthPopuli.com.
Our Mobile Health Data: Shared, Identifiable, and Privacy-Deprived posted first on http://dentistfortworth.blogspot.com
Wednesday 27 March 2019
Having Health Insurance Is A Social Determinant of Health
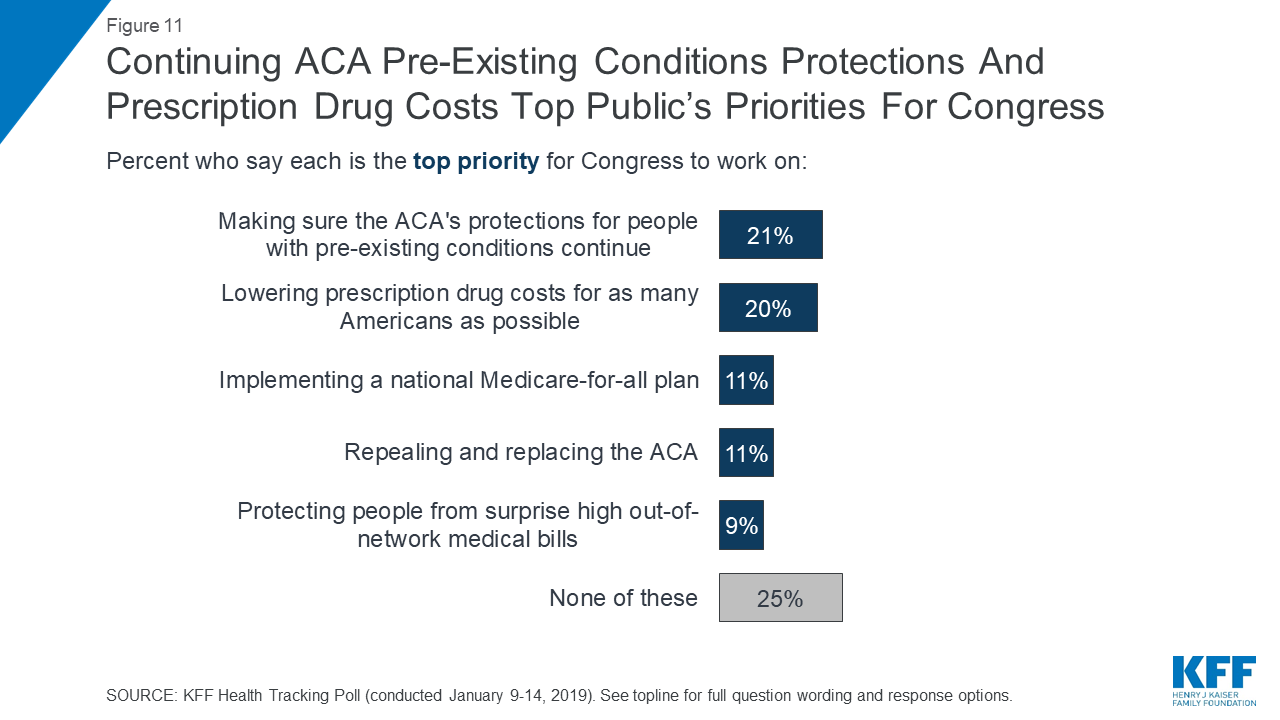
Health insurance was on the collective minds of American voters in the 2018 midterm elections. Health care, broadly defined, drove many people to the polls voting with feet and ballots to protect their access to a health plan covering a pre-existing condition or to protest the cost of expensive prescription drugs. These were the two top health care issues among voters in late 2018, a Kaiser Family Foundation poll at the time assessed.
Yesterday, President Trump verbally re-branded the Republican Party as “the party of healthcare.”
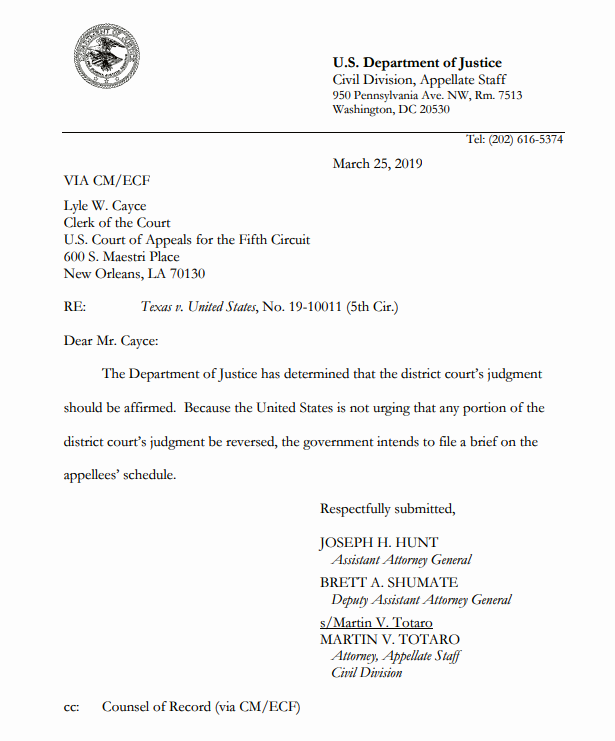 That Presidential pronouncement was tied to a letter written on U.S. Department of Justice letterhead RE: the Texas v. United States case. Two sentences succinctly stated, “The Department of Justice has determined that the district court’s judgment should be affirmed. Because the United States is not urging that any portion of the district court’s judgment be reversed, the government intends to file a brief on the appellees’ schedule.”
That Presidential pronouncement was tied to a letter written on U.S. Department of Justice letterhead RE: the Texas v. United States case. Two sentences succinctly stated, “The Department of Justice has determined that the district court’s judgment should be affirmed. Because the United States is not urging that any portion of the district court’s judgment be reversed, the government intends to file a brief on the appellees’ schedule.”
Texas v. United States was the case brought by state Attorneys General beyond Texas, including Alabama, Arizona, Arkansas, Florida, Georgia, Indiana, Kansas, Louisiana, Missouri, Nebraska, North Dakota, South Carolina, South Dakota, Tennessee, Utah, West Virginia, and Wisconsin, along with two governors from Maine and Mississippi.
The Los Angeles Times reported this story as, The Trump approach to healthcare: Break it and figure out the rest later.
“Break” is an appropriate description, because about 21 million people who finally enrolled in health insurance would lose their benefits. Twelve million people would lose Medicaid coverage. About 2 million young people would also lose coverage, now health-insured under their parents’ health plans. The millions of people covered by employer-sponsored health plans would also be impacted: the ACA baked in assurances for lifetime caps on personal health spending, as well as guarantees for covering pre-existing conditions. Medicare enrollees, too, would face higher payments.
More details on losing stakeholders are covered in this extensive New York Times analysis. which observes, “Nor is the Affordable Care Act some minor statute that can be shoved aside without disruption. It is now part of the basic plumbing of the American health care system.”
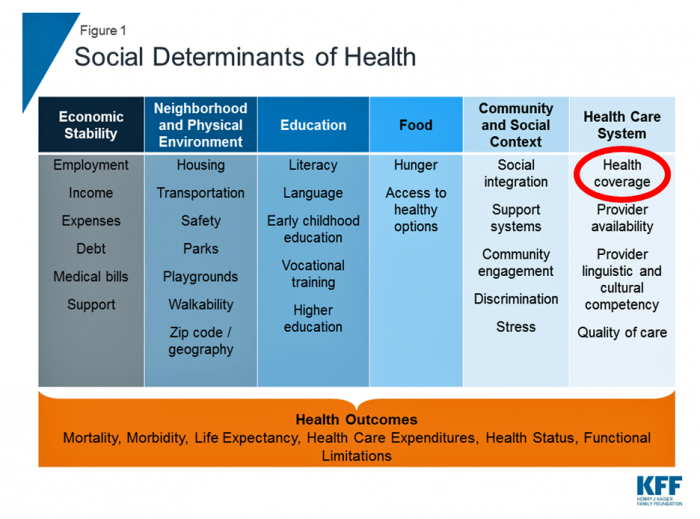 I’ll speak simply. Assuring access to the health care system is a social determinant of health, as the inventory from Kaiser Family Foundation includes in their chart here. Ensuring health coverage is smart, economically, because insurance bolsters peoples’ on-ramp to needed medical services and prescription drugs. That underpins health security, and the economic benefits of productivity at work, ability to seek that job, opportunity to pay (more) taxes, and energy to participate in daily life — social, emotional, financial, and indeed, political and civic.
I’ll speak simply. Assuring access to the health care system is a social determinant of health, as the inventory from Kaiser Family Foundation includes in their chart here. Ensuring health coverage is smart, economically, because insurance bolsters peoples’ on-ramp to needed medical services and prescription drugs. That underpins health security, and the economic benefits of productivity at work, ability to seek that job, opportunity to pay (more) taxes, and energy to participate in daily life — social, emotional, financial, and indeed, political and civic.
Health care insurance and service access are social determinants of health. The healthcare industry has been paying more attention in the past few years to social determinants; especially food and nutrition (through, say, healthy food prescriptions and hospital programs like the Geisinger Food Farmarcy); transportation, with Lyft and Uber playing growing roles in medical transportation filling the mobility gap; and, greater attention to environmental and climate programs, learning from the Flint water crisis and downstream (literally) negative health impacts, along with knowledge about air particulates’ negative impact on respiratory conditions like asthma and COPD.
A strong primary care backbone builds a stronger health care system for all health citizens in the rest of the developed world. Through my health economic lens, I’ve reinforced this in my work and writing, most recently here on Health Populi.
 It’s encouraging to see that health insurance companies have begun to incorporate social determinants services into health plans, increasingly common now in Medicare Advantage plans supporting long-term social supports addressing housing (Kaiser Permanente’s program), loneliness and social isolation (CIGNA’s concept), and transportation (via Lyft’s growing health division working with a range of plans and providers). Interestingly, health insurance stocks took a hit on the markets by the end of day yesterday.
It’s encouraging to see that health insurance companies have begun to incorporate social determinants services into health plans, increasingly common now in Medicare Advantage plans supporting long-term social supports addressing housing (Kaiser Permanente’s program), loneliness and social isolation (CIGNA’s concept), and transportation (via Lyft’s growing health division working with a range of plans and providers). Interestingly, health insurance stocks took a hit on the markets by the end of day yesterday.
Health Populi’s Hot Points: Do I state the obvious here? For some of us who went to school in public health, nursing, medicine, social work, education, it is obvious and even cliché that having health insurance bolsters health.
It’s not so obvious to some public policymakers or voters who have chosen to erode the Affordable Care Act (ACA). Even with the continued paring back of aspects of the ACA, 8.5 million people signed up for ACA marketplace health plans by the December 15, 2018 deadline.
By the end of 2018, a Gallup poll found that most Americans believed that the U.S. government should ensure health care for Americans. I spelled that “ensure,” with an “e.” In the poll, most people also didn’t want the government to run that system. Ensuring health care is making certain people have access to necessary health care. That’s the prevailing opinion in the overall America.
Perhaps this fellow had something to do with keeping enrollment alive for American health care in 2019.
The post Having Health Insurance Is A Social Determinant of Health appeared first on HealthPopuli.com.
Having Health Insurance Is A Social Determinant of Health posted first on http://dentistfortworth.blogspot.com
Tuesday 26 March 2019
Monday 25 March 2019
Are we forgeting about our caregivers?
The New York Times has a very interesting piece on the caregiver experience.
Americans spend so much time debating so many aspects of health care, including insurance and access. Almost none of that covers the actual impossibility and hardship faced by the many millions of friends and family members who are caregivers. It’s hugely disrupting and expensive. There’s no system for it. It’s a gaping hole.
Consider the case of one caregiver helping provide the support a friend needed after receiving a cancer diagnosis.
Every appointment required Jim and Ali to take off work. They live in Indiana, and at one point they had to pay for flights and a hotel room and everything else associated with a trip to New York — none of it covered by insurance — because no one would do the second opinion remotely. (He had a kidney removed in an initial operation, then doctors found he had a rare cancer, a neuro-ectodermal tumor, instead of the expected renal cell carcinoma).
Chemotherapy is rough. After each cycle, Jim would pretty much sleep or rest for a week, unable to work. Someone had to take the time to be with him. Sometimes it was Ali; sometimes it was my wife, or me, or other friends.
Measuring the value of new treatments that improve patients health often focuses on the benefits the new treatment can provide to patients. But curing a disease or significantly reducing its impact on their quality of life not only can transform the patient’s life, but also that of their caregiver as well.
As I wrote two months ago, the impact of a disease or a treatment for that disease on caregiver burden can be quantified. The CarerQoL and the Care Experience Scale (CES). are two such instruments. In fact, the Second Panel on Cost Effectiveness in Health and Medicine recommends incorporating a treatment’s impact on caregiver burden as part of any value assessment conducted from a societal perspective.
In short, caregiver’s are health care’s unsung heroes and the value of new treatments to free up their time should now be ignored.
Are we forgeting about our caregivers? posted first on http://dentistfortworth.blogspot.com
5 Fun Tips to Tame Kids’ Temptation for Sweets
Sweet treats…a temptation for both children and parents (if we’re honest).
Would you be surprised if we started by reminding you that children love sweets?
Of course not! There’s even scientific evidence out there that shows children don’t just like sweets, they’re biologically hardwired to them.
Julie Mennella of the Monell Chemical Senses Center explains in recent research, “the newborn can detect sweet acutely, and will actually prefer sweeter solutions to less sweet ones. The basic biology of the child is that they don’t have to learn to like sweet or salt. It’s there from before birth.” Monella’s research also demonstrated that sugar helps children tolerate pain, and that it’s a natural pain reliever for them (wow)!
On the other hand, sweet treats are also tempting for parents to use as rewards for their children’s good behavior. Although it’s seemingly the quickest and easiest way to reward your child and will definitely earn a few smiles, there’s a catch here. By using sweets as a reward, we risk building a bad habit for kids because we teach them that sweets can be better than others (by merit of the fact they’re seen as a “special reward”).
We come by our sugar fix naturally, but consuming too much can have shocking effects on your child’s oral and overall health. In this article, we’re going to talk about the dangers of sugar, yes, but (more importantly) the ways to simply cut down the sweets intake (and cravings) of your child.
First things first—how much sugar is OK?
The American Heart Association (AHA) recommends that children between 2 and 18 years old should all eat less than 25 grams—or six teaspoons—of added sugars daily. And yes, we are talking about refined sugar, not the natural sugar you find, say, in broccoli.
The AHA goes on, “Children and teens should limit their intake of sugar-sweetened drinks, specifically, to no more than eight ounces (or one glass) weekly.”
These recommendations also advise that children under the age of two should have no added sugars at all.
The same AHA publications also drops the handy reminder that the estimated volume of calories a child needs ranges from 1,000 a day for a sedentary two-year-old to 2,400 for active 14-18 years old girls and 3,200 for active 16-18 years old boys. Check the sugar content on foods and drinks, because it will have a direct impact on the number of calories consumed.
According to Miriam Vos, M.D., Ms.P.H, “if your child is eating the right amount of calories to achieve or maintain a healthy body weight, there isn’t much room in their food ‘budget’ for low-value junk foods, which is where most added sugars are found.”
Sweet treats and sugary drinks are rich in calories at the same time that they’re poor in nutrients. Most added sugars can be found in sodas, energy and food drinks, cookies and cakes, ice cream, candies, and other desserts. And no, those don’t form part of the food pyramid.
Consuming foods high in added sugars at a young age has also been linked to other risk factors such as increased risk of obesity, elevated blood pressure, diabetes, dyslipidemia and, of course, tooth decay.
How sugar affects oral health
You (and even your kids) already know that too much sugar will affect oral health. But let’s take a look at the “why.”
To begin with, sugar itself is not the issue, rather what happens after consuming it. Our mouths are full of bacteria, many of which are beneficial to our oral health. When we consume too much sugar, however, the “naughty” bacteria will use it as a fuel and break it up, thus producing acids. These acids will then stick and start dissolving the minerals that make the enamel, which is the protective layer of our teeth.
This “feeding” on the enamel will result in cavities and tooth decay.
How to (realistically) cut back on your child’s sweets consumption
With all those delicious temptations a breath away, and provided that children are biologically hardwired to love sweets, cutting back on candies can be a daunting task for many parents and caregivers. However, the health benefits will be long-lasting and definitely worth the effort.
We even have a list of tips to make the process easier. How’s that sound?
1: Make fruits the first choice to “satisfy sweet”
Fruits can be as delicious as sweets, especially after a short adjustment period where the palette “resets” to natural sugars (at which point fruit naturally tastes sweeter). Plus, fruits are packed with vitamins and nutrients essential for your child’s growth. As if you needed more reason, they also have fewer and healthier calories than foods with added sugar. And last but certainly not least, there is even a connection between a child’s low-quality diet (without fruits) and performance at school.
So, to make more fruit-eating happen:
- Always keep fruits in sight in the kitchen
- Have a variety of fruits available
- Find ways to play with your child using fruits (for example, you can create structures by cutting fruits into fun and easy shapes such as snowmen and funny faces—yes, please play with your food)
- Invent new snacks with fruits (like a fancy fruit salad with a cool name) and prepare them with your child on a regular basis
2: Don’t offer sweets as rewards
As mentioned earlier, the easiest way to reward your children seems to be by offering them sweets. However, you build a bad diet as well as bad habits for children by doing this because you ultimately teach that sweets are more exciting than healthier foods. Consider rewarding your child with something like an activity, hugs and kind words. In addition, you can give your child other no-food rewards like stickers or drawing tools.
3: Drink responsibly!
Sugar-sweetened drinks such as soda contain a lot more sugar than you realize, and they are also high in calories and low-to-nothing in what they offer in nutrition. When your children are thirsty, give them water (and set the crucial example of drinking more of it yourself).
4: Keep sweets for special occasions
If we’re honest, it’s realistically OK for your child to eat candies on Halloween or other special days. Let your child enjoy them, and link candies and other sweets only to special occasions such as Halloween. You don’t have to worry about one day of the year, or even two or three, but you should be careful about the rest. If your child asks for some candy on non-special days, you can consider some, but only in small portions.
5: Be creative with snacks
Healthy foods may not look as fancy or enticing as candies and sweets. However, with just a bit of creativity, you can make your children love their new snacks! Bright colors and exotic textures can do the trick, both of which are abundant in the world of fruits and veggies.
And back to an earlier idea, you can also play games with healthy foods (gamification, we call it these days), such as encouraging your child to find the amount of total sugars on the Nutrition Facts label in foods to compare them with healthy foods they like. Or how about an apple tasting? Or letting your kids pick out the fruits in the grocery store for the fruit salad party at home?
Cutting down your children’s consumption of sweets might look like a tough task. However, the long-lasting health benefits are without a doubt worth the effort. So, arm yourself with patience and a little bit of creativity, and remember that it’s about progress today, not perfection!
The post 5 Fun Tips to Tame Kids’ Temptation for Sweets appeared first on Fort Worth Dentist | 7th Street District | H. Peter Ku, D.D.S. PA.
5 Fun Tips to Tame Kids’ Temptation for Sweets posted first on http://dentistfortworth.blogspot.com
Sunday 24 March 2019
How easy is it for ICER to predict budget impact?
The answer–according to a recent study by Thornton Snider et al. (2019)–is not that easy. Using case studies of ICER report’s predictions of unmanaged uptake of new medications before 2016, the paper estimates how well these reports predict price, uptake, and overall spending. The authors find:
ICER’s uptake estimates exceeded real-world estimates by factors ranging from 7.4 (sacubitril/valsartan) to 54 (hepatitis C treatments). The “unmanaged uptake” assumption (removed from ICER’s approach in 2017) yields large deviations between BIM estimates and real-world consumption. Nevertheless, in some cases, ICER’s BIMs that relied on current market estimates also deviated substantially from real-world sales data.
Overall, ICER’s price estimates were not too far off, typically 15%-24% higher than actual prices. However, the unmanaged uptake assumption meant that utilization estimates were off by 2500% for new drugs and even by 760% for drugs already in the market. Combining these affects, total spending on these medications was overestimated by a factor or 36 for new treatments, and by a factor of 8.6 for drugs already in the market.
Source:
- Snider JT, Sussell J, Tebeka MG, Gonzalez A, Cohen JT, Neumann P. Challenges with Forecasting Budget Impact: A Case Study of Six ICER Reports. Value in Health. 2019 Mar 1;22(3):332-9.
How easy is it for ICER to predict budget impact? posted first on http://dentistfortworth.blogspot.com
Friday 22 March 2019
Weekend links
- Thoughts on IPI.
- Thoughts on suicide.
- Where is California workers’ comp headed?
- What’s next for FDA?
- Vitale: Just pay the players.
Weekend links posted first on http://dentistfortworth.blogspot.com
Thursday 21 March 2019
Isn’t It Eyeconic? Vision Care in the Evolving Health Care Ecosystem
The vision/optical industry is one piece of the health/care ecosystem, but the segment has not been as directly impacted by patients’ new consumer muscles until just about now.
 It feels like the vision industry is at an inflection point at this moment, I intuited during yesterday’s convening of Decoding the Consumer: The new science of customer behavior, the theme of the 13th annual global leadership summit hosted by Vision Monday, a program of Jobson Medical Information which is part of the WebMD family.
It feels like the vision industry is at an inflection point at this moment, I intuited during yesterday’s convening of Decoding the Consumer: The new science of customer behavior, the theme of the 13th annual global leadership summit hosted by Vision Monday, a program of Jobson Medical Information which is part of the WebMD family.
I was grateful to have an opportunity to share my views with attendees on the vision patient as health consumer through the health economic lens.
Marc Ferrara, CEO Information Services with Jobson, introduced the meeting with some context. The topic, “decoding the consumer,” was chosen as that vision patient, now consumer, has growing control over their experience – as they seek services for vision care and shop for products (lenses, eyewear, and supplies).
This is impacting optical retailers, from the corporate giants to the still-large presence of Mom-and-Pop brick-and-mortar storefronts in shopping strips, mega-malls, and even practitioners’ homes in exurban and rural geographies.
There’s a new data continuum with a shift in the relationship between the deliverers of services and their buyers. That data powers new relationships and programs, Marc explained.
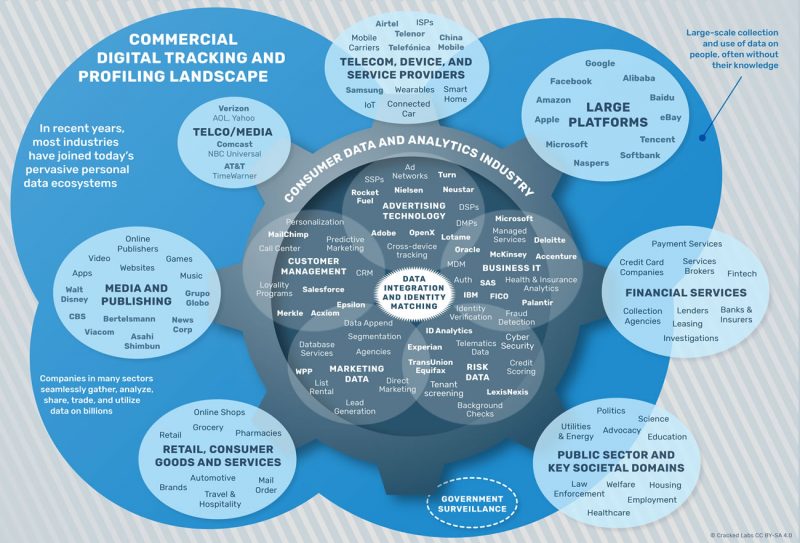
He shared this image from Cracked Labs which illustrates the many data sources beyond the legacy health care claim that stakeholders can access and, if used for good, can benefit patient care and health outcomes.
Marc then presented an intriguing, if disturbing (to me), bar chart of “the future value of your data.” Globally, that calculated to a value of $2.36 per average internet user per month in 2025, $3.18 for the European citizen, and a whopping $9.82 for Americans. There are reasons underneath this value-calculation I’ll address in another post: top-line for me is Americans’ lack of comprehensive data privacy protection and lack of opt-in to data collection in everyday life (addressed in the concluding Hot Points, below).
In addition to the “data is the new oil” mantra, Marc noted the growth of omnichannel in retail that has begun to re-shape the consumer-facing optical industry. Over one-half of 213 retail chains listed in Internet Retailers top 1000 offered “buy online, pick up in store” fulfillment in 2018. Walmart, in particular, had a huge uptick in this during the 2018 holiday shopping season.
Marge Axelrad of Jobson then set out the agenda for the day, asking one of the day’s big questions, “Can experience and data co-exist?” She said, “of course it can,” as the day’s content proved out.
”We’re a little bit value and a little bit luxury” these days, Marge observed.
“Data and tech can re-define new experiences,” she said. We’re relying on technology to help us learn about what best works for consumer experience. And that’s true for health care as well as generic retail, Marge asserted, introducing Deborah Weinswig who is CEO and Founder, Coresight Research. Deborah spends one-third of her time in China, these days, and gave us the benefit of her learnings from Asia and retail innovation.
Technology is re-shaping physical retail, from Tiffany and Nike to retail pharmacy. Tech integration in the store and via e-commerce is changing the customer experience — and experience is table stakes now to keep the consumer’s loyalty, which is increasingly fleeting.
Here, Deborah’s concept of “boundaryless retail” will be quite relevant for health/care stakeholders, as the consumer can and will seek health everywhere – at home, on the go at grocery stores and workplaces, in their cars…omnichannel beyond (but including) media platforms.
Frictionless retail is also an important paradigm for health care, an industry rife with friction. A huge friction point we identified in our data-for-healthcare-good panel wrapping up the day is surprise medical billing due to patients’ unwitting use of out-of-network physicians and providers. Blockchain is proving to be a sound, effective use-case for keeping provider directories and credentialing up-to-date.
And that will enhance patient/consumer health experience and loyalty.
AI underpins all retail experience now – which is something we’re hearing in healthcare whether at HIMSS, CES, SXSW, ePharma, and other conferences since the start of 2019.
My talk was next up, as I presented the evolving retail health/care ecosystem landscape and the growing role of the patient-as-payor.

Andy Karp of Jobson kicked off the afternoon’s content which focused on data and technology. When Andy spoke of us all being part of the “digital nation” as “digital citizens,” his remarks resonated with me. “We are all part of the digital nation….we pledge allegiance to the digital nation several times a day,” he waxed lyrically. “The only passport we need is a smartphone.”
That means we need a code of data ethics, and for that Andy cited Accenture’s report on Building Digital Trust with 12 principles for using data for good.
A panel on the promises of blockchain technology for health care brainstormed how to make data more transparent, more secure, and more accessible for everyone in the data sphere, with Jill Malandrino of NASDAQ parrying with Janine Grasso of IBM’s blockchain team, and AdventHealth’s CTO Roger Smith bringing his in-depth health system knowledge to the insights.
I believe that the health care industry can learn from IBM’s “journey of a mango from farm to retail,” as Janine described, using blockchain to trace a food chain from farm to fork. Her experience in the early days of blockchain-building across all industries is that 20% is the hard initial work, but 80% of the project is convening the network to agree governance and incentive structures.
IBM is building a Health Utility Network which includes Aetna and Anthem, among other partners, to use for credentialing, claims processing, and other services.
Dr. John Whyte, Chief Medical Officer with WebMD, spoke about how people use the internet for health care search. As a Board Certified Internist, Dr. Whyte speaks as both a front-line health care provider in Washington, DC, as well as through his lens on the inside of WebMD, still among the most-trusted healthcare information portals: one in four U.S. adults uses WebMD each month, and the site is #1 in reach for the top 50 diagnosed conditions, he noted.
It’s also the #1 health site for eye glass wearers 25-54 years old. Over 20 million info seekers on WebMD had an eye exam in the past twelve months. Top search terms for vision/optical information were for dry eye (39%, and weighted toward women seeking this answer), astigmatism (34%), myopia (29%) and floaters/flashes (24%).
People have a lot of curiosity about eyes, John observed — what does an eye color say about one’s health? How can I banish bags from my eyes? What causes eye pain? The questions are many and varied and curious.
No health conference is well-curated in 2019 without some discussion on the growing role of voice tech, and Dave Bovenschulte, VP Strategy with Klick Health, and Justine Santa Cruz, SVP with Satisfi Labs, brought their deep knowledge to the topic. Their remarks informed our last panel session on turning data wealth into patient health.
Amy Heymans (Cueva), founder and leader of Mad*Pow (one of my own go-to health/tech designers) spoke on design for health care, patient engagement and behavior change; and John Ryan, General Manager of UnitedHealthcare Vision spoke of his organization’s strategic use of data in patient care programs for vision health.
Our end-of-day panel featured Dr. Whyte and me synthesizing the findings of the day on how health care and, especially, the vision/optical industry, can leverage data to benefit patient care and health. The elephant in the room all day, I felt and said, was privacy — or lack thereof. While Europeans in the room — remembering two of the major sponsors of the meeting were Essilor (based in France) and Luxxotica (based in Italy) — are covered by the GDPR for privacy of personal data, Americans are barely covered by a patchwork privacy quilt of HIPAA, GINA, COPPA (for children online), and other bits of policy. But the non-traditional data bytes (detailed in the Cracked Labs graphic above) that industry, and especially retail at large, are mashing up aren’t usually covered by HIPAA, unless they reside in HIPAA-covered entities’ information systems.
Our group-of-seven crowdsourced the importance of trust, transparency, and data stewardship to ensure that the patient-as-health-consumer and, ultimately citizen (in my own view) benefit from sharing data. Without these values and an ethical data framework, people won’t fully engage in health care…to the detriment of individual and public health.
Health Populi’s Hot Points: As experience and service become mantras in health care @ retail, it’s useful to call out a recent announcement from VSP, among the largest eyecare insurance providers.
 You know about CVS buying Aetna late last year, bringing together the pharmacy-cum-healthcare services operation with a health insurance plan.
You know about CVS buying Aetna late last year, bringing together the pharmacy-cum-healthcare services operation with a health insurance plan.
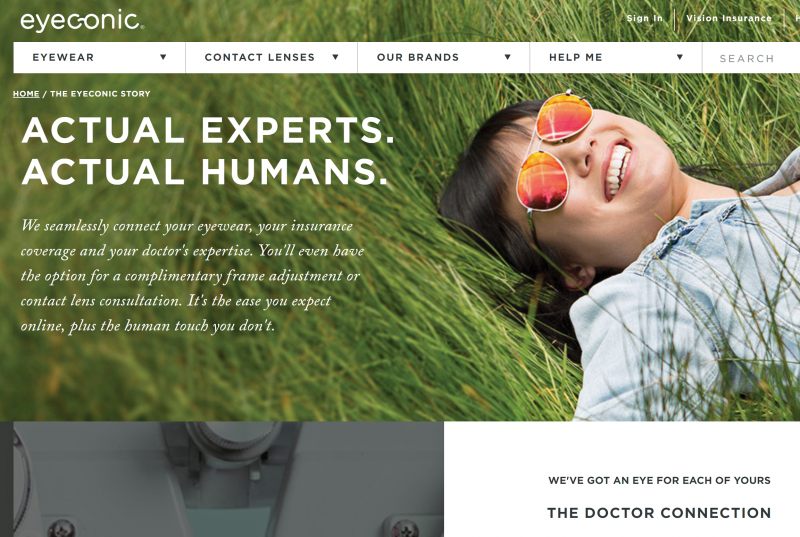
Now consider a vision/optical insurance plan entering the retailing side of the business. This is the news coming from VSP, one of the largest providers of vision insurance covering 88 million members, launching its retail optometry business cleverly named Eyeconic.
In their online story, they tout the tagline, “Actual Experts. Actual Humans.”
Check out the lower right portion of the website snippet: “We’ve got an eye for each of yours…The Doctor Connection.” A key message of Eyeconic is their value proposition of connecting you, the patient-consumer, with a real-living doctor, not a chatbot, an app, or virtual human.
As I reflected on Eyeconic and what it means for the vision consumer, I told the group about Dr. Eric Topol’s latest book, Deep Medicine (reviewed here in Health Populi). The tag line of the book is how AI can help humanize health care.
The message here that Eyeconic has adopted meshes with Dr. Topol’s view that AI is key to helping humanize health care — but to complement and enhance the provider’s ability to spend quality time in partnership with patients.
The post Isn’t It Eyeconic? Vision Care in the Evolving Health Care Ecosystem appeared first on HealthPopuli.com.
Isn’t It Eyeconic? Vision Care in the Evolving Health Care Ecosystem posted first on http://dentistfortworth.blogspot.com
How long will you wait for cancer treatment in the UK?
How long does it take to get treated for cancer in the United Kingdom’s National Health Service (NHS)? How long does it take for ambulances to arrive? What about wait times at ED visits?
An article in The Independent answers these questions with statistics from NHS itself. The answer to the above questions, about 1 in 5 people will wait for more than 2 months between being diagnosed with cancer and receiving treatment. Ambulances generally only take 7 minutes for the most severe emergencies but take over 23 minutes for less severe cases. About one in six patients requiring emergency department care will wait more than 4 hours before being treated, admitted, or sent home.
So what is the NHS to do? Set new targets to lower wait times? Well actually they have done the opposite; they are scrapping wait time targets. While this may seem like a perverse response, I am actually supportive of the move. Tracking wait times is important but fixed targets may create perverse incentives. For instance, there may be an incentive to reduce wait times for marginal patients who physicians can move below the target; for patients already past the target, physicians may de-prioritize their wait times. In fact, there is some suggestive evidence for gaming the system:
Around one-fifth of emergency admissions occur in the 10 minutes before the four-hour window would have been breached – suggesting clinical decision making is being sidelined by the limit.
The targets may also reduce staff morale. In short, although reducing wait times in the NHS is important, instituting top-down, overly-simplistic, bureaucratic wait time targets are not the way to go.
How long will you wait for cancer treatment in the UK? posted first on http://dentistfortworth.blogspot.com
Tuesday 19 March 2019
The Evolution of Self-Care for Consumers – Learning and Sharing at CHPA
Self-care in health goes back thousands of years. Reading from Hippocrates’ Corpus about food and clean air’s role in health sounds contemporary today. And even in our most cynical moments, we can all hearken back to our grandmothers’ kitchen table wisdom for dealing with skin issues, the flu, and broken hearts.
The annual conference of the Consumer Healthcare Products Association (CHPA) convened this week, and I was grateful to attend and speak on the evolving retail health landscape yesterday. Gary Downing, CEO of Clarion Brands and Chairman of the CHPA Board, kicked off the first day with a nostalgic look back at his father’s truck, which motored between mom-and-pop stores in Dad’s work as a “rack jobber.” This was a family business run by mom and dad, started after World War II. Dad owned the “rack” in his clients’ stores and filled that shelf with whatever over-the-counter products the store needed replacing based on shoppers’ demands.
Gary looked back at that era, realizing his father’s understanding of consumer needs at retail. Then Gary looked forward at the evolution of self-care – the theme of this year’s annual conference.
Since George Washington curated a list of medicines for his troops, in search of tinctures and oils for dealing with the harsh environment and challenging battlegrounds, to today’s challenges of ecommerce and new products like CBD oils disrupting today’s marketplace, the concept of self-care continues to evolve.
Key issues facing the industry in 2019 and into the next few years range from regulation of dietary supplements and the role of CBD in self-care, the omni-channel consumer, ecommerce vs. bricks-and-mortar, trust, and wrestling with consumer privacy.
 To meet the future, Scott Melville, CEO of CHPA, described the organization’s 2020 project which is determining the categories the Association should represent. Remember that the CHPA has a 138-year old heritage. For the organization’s 2020 vision, there are three category pillars in sight: over-the-counter (OTC) drugs (the core mission for over a century), dietary supplements, and consumer medical devices (think: the CES digital health aisles, and beyond).
To meet the future, Scott Melville, CEO of CHPA, described the organization’s 2020 project which is determining the categories the Association should represent. Remember that the CHPA has a 138-year old heritage. For the organization’s 2020 vision, there are three category pillars in sight: over-the-counter (OTC) drugs (the core mission for over a century), dietary supplements, and consumer medical devices (think: the CES digital health aisles, and beyond).
Among Scott’s many insightful comments, one really resonated with me and my health-economics mindset: on the growing presence of value-based insurance design in the U.S. Scott called out the work of Nicholas Bagley at University of Michigan (my alma mater – Go Blue!). The goal of VBID is to align costs and outcomes in health care in terms of paying for what brings value. “Value-based insurance design is the holy grail, at least for new drugs,” Nicholas was quoted in the New York Times. “But we wouldn’t want to pay a value-based price for aspirin. Doing so would cause us to pay a lot more for it than we do today.”
The point here is that private-label aspirin costs about five cents per tablet. But the value that little pill brings to a person-patient-consumer-payor is much greater than a nickel.
“Does that mean that politicians and consumers will argue they should cost more?” Scott rhetorically asked.
Well, no, Scott pragmatically answered.
The point is that the consumer healthcare industry has to do a better job communicating the value provided by these products.
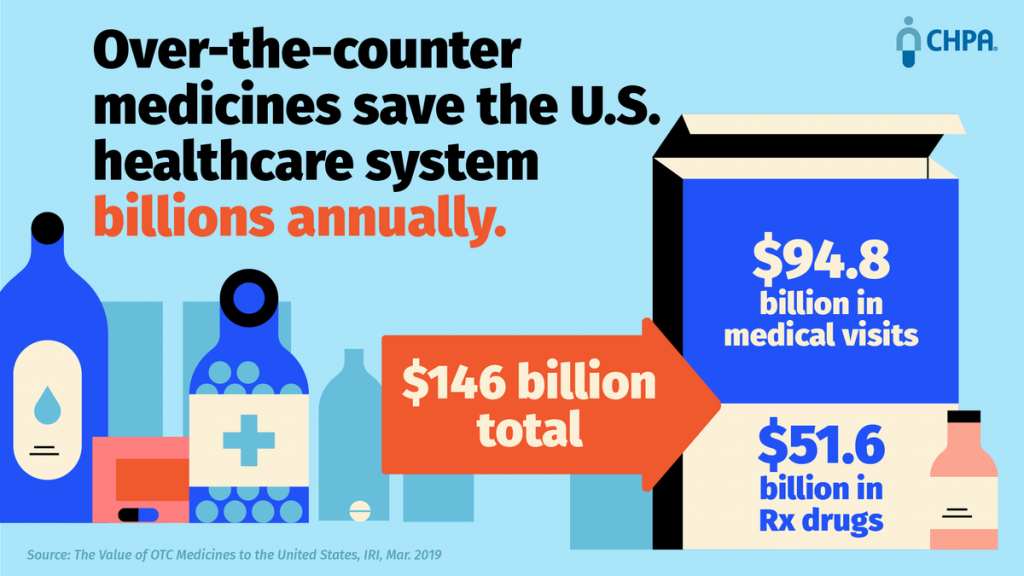
CHPA released a new study this week into the value of OTC meds. The report calculates that these products save the U.S. health care system $94.8 billion in medical visits and reduce reliance on prescription drugs by a $51.6 billion savings. That totals $146 billion. The bottom line: each dollar spent on OTCs saves over $7 in the U.S. medical system in terms of direct costs.
Indirect costs are an additional layer of value: for companies, workers using OTC meds generate $34 billion in workplace productivity benefits. Payors have begun to recognize the value of nudging consumers toward over-the-counter products under Medicare Advantage plans. For example, Anthem and Walmart introduced the Healthy Benefits program, a card that covers $50 to $330 of OTC spending per quarter depending on the plan.
Here’s a video that talks about some of these findings – with the tagline, “Don’t waste your day feeling sick. Use your sick days for more serious stuff.”
 Next up in the agenda was the presentation of the Ivan D. Combe Lifetime Achievement Award. You know Combe and his family’s company by the helpful, engaging brands they’ve brought us over the years like Just for Men, Seabond, and Vagisil. It’s this last brand that sponsored the reception and public launch of the WE initiative to support the professional growth and sustainability of female leaders in the consumer healthcare industry. Keech Combe Shetty, granddaughter of Ivan and Co-CEO of Combe, bolstered the importance of women’s leadership in the health care industry as both a role model and supporter. If you follow the Vagisil brand and others in the Combe portfolio, you will see the company’s support of women’s health, engagement and empowerment.
Next up in the agenda was the presentation of the Ivan D. Combe Lifetime Achievement Award. You know Combe and his family’s company by the helpful, engaging brands they’ve brought us over the years like Just for Men, Seabond, and Vagisil. It’s this last brand that sponsored the reception and public launch of the WE initiative to support the professional growth and sustainability of female leaders in the consumer healthcare industry. Keech Combe Shetty, granddaughter of Ivan and Co-CEO of Combe, bolstered the importance of women’s leadership in the health care industry as both a role model and supporter. If you follow the Vagisil brand and others in the Combe portfolio, you will see the company’s support of women’s health, engagement and empowerment.
Timothy Hayes was given the Combe Award for his many years in the consumer health business. Interestingly, importantly, I noted that Tim began his career at Quaker Oats. I found this intriguing due to the consumers’ increasing engagement with food-as-medicine, which featured prominently in IRI’s research discussed next at the conference.
To that point, IRI’s Kristin Hornberger presented new data on retail health market performance in 2018. “It’s challenging out there,” she began, with store growth at only one to two percent in the year. “We have to get better at reaching consumers and shoppers,” Kristin recommended.
Consumer health as a category was $45 billion in 2018, growing at 2.1%. Prescription drug growth at retail was 5.5%, so consumer health lagged. Some specific consumer health brands and categories were faster-growing than others: Garden of Life, Sambucol, Pedialyte, Nature’s Truth, among them.
Nutritionals had a rebound after a slower 2017, growing 4.2% in 2018. In contrast, healthcare excluding nutritionals grew only 1.5%. What has been driving nutritionals growth is consumers’ interest in managing disease states, focusing on bolstering immunity, brain health, beauty, protein and meal replacement, and managing Inflammation.
Kristin unpacked the trend, noting three key factors underneath consumer health’s slow growth in 2018: a less severe cold and flu season, limited product innovation in 2018 (with virtually no Rx to OTC switch), and a growth of private labels outpacing more expensive brands for vitamins, sleep aids, antacids, support devices, and first aid.
But there are green shoots for consumer healthcare retail growth in 2019: the exploding sales of CBD and hemp-based products; greater self-care among consumers, with 34% more people actively practicing more care at home over the past year; and, brands taking a stand for sustainability, responsibility, and community support (think: TOMS and Warby-Parker coming to consumer products and health/care retailers).
As an example, Kristin pointed to the Tylenol #WeCare campaign, shown in this video:
IRI’s Nishat Mehta tag-teamed with Kristin, discussing the growth and importance of influencer campaigns and new marketing modes. Nishat noted that the “death of television” discussed in mass media is highly over-rated. In fact, media is fragmenting, but TV has mass scale when strategically used. “It’s an ‘and,’ not an ‘or,’” Nishat believes, in terms of being where the consumer is: which is very often streaming TV.
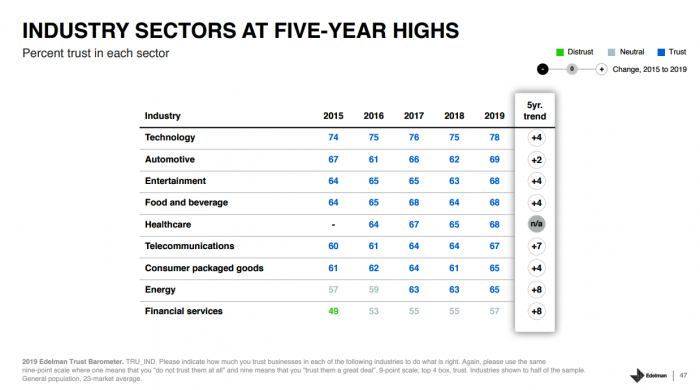 Edelman followed IRI’s informative session, discussing one of my favorite studies each year: the Trust Barometer, which I wrote about in January 2019 discussing this year’s finding that the Employer is the most trusted organizational touchpoint among global consumers. This is an important shift away from trusting “people like me” and peers – as Employers are engendering a sense of familiarity with authority (for facts and information), explained Jenn Hoker.
Edelman followed IRI’s informative session, discussing one of my favorite studies each year: the Trust Barometer, which I wrote about in January 2019 discussing this year’s finding that the Employer is the most trusted organizational touchpoint among global consumers. This is an important shift away from trusting “people like me” and peers – as Employers are engendering a sense of familiarity with authority (for facts and information), explained Jenn Hoker.
I was particularly keen to take in Courtney Gray Haupt’s presentation of data through the lens of healthcare, which will be published in full soon. I’ll cover that in detail, as I did last year in Health Populi.
The growth in health care trust was 8 points up this year, an impactful finding in that in 2018, there was a plummet in trust for health care. Globally, health care trust hit 67, and in the US, 61.
Edelman’s health industry segments for this study are pharma, consumer health, insurance, biotech/life science, and hospitals.
U.S. consumer trust across all of these segments increased – except, surprisingly, for hospitals, which fell 7 points. Consumer health went opposite, up 7 points, biotech up 3, insurance up 8, pharma up 6.
Peter Segall rounded out the Edelman trio, providing a larger context for health companies to consider in their communications strategies. He noted that 56% of consumers trust media on consumer health, but 66% trust the credibility of information from health companies.
“Tell your health tech story,” Peter urged. Consumers are “Missourian” in that they want industry to show they the data and research on a personal level. “People need to impute personal benefits,” he explained, encouraging us to, “know your audience…and know how your audience knows you.”
Ultimately, the objective must be to be transparent and balanced in every way, especially in using medical data.
My talk on the evolving retail health landscape immediately followed the Edelman panel. Through the health economic lens, I discussed the patient morphing into a consumer and payor, and what that portends for the consumer health/care industry in terms of opportunities and threats. In particular, health@retail does indeed require transparency and respect for a person’s values in a growing value-based environment. We should be mindful that with the patient-as-payor, value means understanding what mainstream people value. And we must communicate that value on a personal basis to that N=1 consumer in health.
The post The Evolution of Self-Care for Consumers – Learning and Sharing at CHPA appeared first on HealthPopuli.com.
The Evolution of Self-Care for Consumers – Learning and Sharing at CHPA posted first on http://dentistfortworth.blogspot.com
HHS recommendations to reform the health care system
HHS has a policy paper titled “Reforming America’s Healthcare System Through Choice and Competition“. In the paper, HHS describes four broad areas of reform. I describe each in term, some of the key policy recommendation under each of the four headings, and my thoughts on each reform. Here goes:
- Health care workforce and labor markets. Here HHS makes a number of wise recommendations. The first is to allow specialties to practice at the top of their license. This means granting non-physician clinicians (e.g., physician assistants, nurse practitioners, dental hygenists) more leeway. HHS also recommends increasing provider mobility by allowing easier transfer of board licensing across states. The out-of-state issue is particularly relevant for telehealth, since it would preclude physicians from practicing ‘out of state’ if the patient is calling in across state lines. Additionally, it makes a lot of sense to modify any reimbursement policies that prohibit or impede alternatives to in-person services. To increase supply (and thus competition), HHS recommends making licensing of foreign trained physicians easier as well.
- Health care provider markets. HHS wisely recommends limiting certificate of need (CON) laws, which have done little to improve quality, but a lot to drive up costs, as well ending or puting more limits on non-compete clauses, which also reduce competition.
- Health insurance markets. HHS recommends ending requirements for “any willing provider”. On the one hand, eliminating AWP will drive down costs because the health plan is restricting access. On the other hand, if the HHS plan aims to increase choice, clearly eliminating AWP do limit patient access to a smaller set of providers within their network. HHS also proposes loosening state regulation of network adequacy standards…again this would drive down cost but decrease choice. HHS also proposes fewer mandates on what should be covered. Generally, this does make sense; some additional flexibility to provider insurance offerings may be helpful in theory. In practice, however, insurance contracts are very difficult to understand and having an essential benefit package makes it easier to shop across plans. Thus, if the essential benefits package is set at a fairly reasonable level, then I would argue it makes sense to keep. In practice, however, lobbying may push Congress to continue to include more and more health care goods and services in the essential benefits package, so I do recognize that there is long-run risk of costs rising due an overly generous benefits package.
- Consumer-driven health care. HHS argues for more high-deductible health plans (HDHP). As an economist, I am partial to these arguments. Insurance causes moral hazard. HDHPs shift cost back to consumers and allow them to better shop. Empirical evidence, however, shows that while people do reduce spending in an HDHP, they also scale back on preventive and high-value care and high-value drugs as the do on lower value care. HHS does make the case that certain high-value treatments (e.g., insulin for diabetics, vaccines), could be allowed to be covered with no cost sharing, which is a more sensible approach. Still, to date, HDHP seem to work better in theory than practice. I do agree, however, with the HHS calls for increased price transparency; it is hard to measure value if one doesn’t know the price being paid. HHS also supports having the government collect quality measures and not overly burdensome, but recommends pivoting away from provider value-based purchasing system, as they are two burdensome, too crude, and sacrifice unmeasured quality for measured quality; I agree. They also propose limiting the use of accountable care organizations. While integrated care with ACOs can work and has worked largely in pilot studies, to date most integration of physician and hospital practice is for the purpose of improving provider bargaining power rather than quality of care provided to the patient. Finally, HHS recommends improving access to claims and electronic medical record (EMR) data from public payers; as a researcher, I couldn’t agree more that better access to data is key to unlocking more insights and better improving the health care system.
In short, while I don’t agree with all the proposals put forward by HHS, there is a lot to like. More choice and more competition are a step in the right direction.
HHS recommendations to reform the health care system posted first on http://dentistfortworth.blogspot.com
Monday 18 March 2019
What You Don’t Want To Read, But Need To See, About Smoking And Your Mouth
The American Dental Association posted a recent video that many won’t want to see, but must—the negative health issues (including fatal oral health complications) that smoking can produce.
The ADA’s video mixes vital facts with gripping visuals to amplify our understanding of the dangers of smoking in the only format many of us are impressed by anymore—video.
The effects of smoking on your oral health goes beyond yellowing of your smile; it causes serious complications, including the very real possibility of oral cancers.
Oral cancer can be aggressive and spread quickly due to the number of blood vessels in your head and neck along with the proximity to your lymph nodes. And while the use of tobacco has been on the decline in the last 20 years, approximately 15% of all Americans still smoke.
Smoking’s effect on the mouth
For many of us, the first thing we notice when someone smokes is the yellow tint to their teeth. The yellow “cooling” is caused by chemicals found in cigarettes that stain the enamel of the teeth. Enamel is one of the hardest substances in the body; however, once it is damaged or eroded, there is no bringing it back.
Infected and receding gums are another sign of a smoker. Smokers are twice as likely to suffer from gum disease as nonsmokers. When the gums are damaged, they can pull away from the teeth and cause the bones underneath to deteriorate. And once the bones break down, it causes instability in the teeth and can cause them to become loose and fall out. This is why many smokers are lacking at least one tooth.
Finally, smoker’s breath is another adverse effect of smoking that virtually all of us are familiar with. Particles from the cigarette are transferred to the mouth where they remain long after you put out the cigarette. These particles can dry out your mouth, which causes bacteria to multiply. The common lack of salvia among smokers spurs this bacteria to attach to the teeth and gum line, too, which is how periodontal diseases are caused.
The most severe complication that can occur due to smoking is oral cancer. It is estimated 80% of those diagnosed with oral cancer are also smokers. Early symptoms of include swelling or lumps around your mouth, red or white lesions in your mouth, and numbness and trouble moving your jaw when talking or eating. If you are experiencing any of these symptoms, it is important you seek medical care immediately.
Electronic cigarettes and smokeless tobacco
Even though you aren’t “smoking it,” smokeless tobacco can still cause significant oral health problems. Just like cigarette smokers, those who use smokeless tobacco are still plagued with bad breath, teeth discoloration and a greater risk of developing periodontal diseases. In fact, smokeless tobacco can increase the risk of periodontal disease even over the rates seen in cigarette smokers. Those who use smokeless tobacco need to visit their dentist more frequently, since oral lesions and other complications can develop quickly and become serious if left unchecked.
Electronic cigarettes are another popular option for people who want to still have the feeling of smoking but—supposedly—without the same concoction of chemicals, and sometimes without the nicotine. These devices have received quite a bit of attention as health professionals determine if they are harmful.
And while these products do have the potential to reduce tobacco use, it is important to remember that no product you inhale is guaranteed safe. Using e-cigarettes can still bring your mouth into contact with nicotine. This can reduce blood flow to the mouth and cause tissues to lose oxygen and nutrients. And when blood vessels contract, it can cause gum line recession and all the other symptoms of chronic cigarette smoking. E-cigarette use can also lead to dry mouth, which allows bad bacteria to multiply and result in cavities or other infections.
If you choose to use e-cigarettes to transition away from smoking, it is important you tell your dentist and continue to go to your regular appointments. Your dentist will be able to spot signs of periodontal disease.
Any time you are inhaling a product—tobacco laced or not—there is the potential for harm to the mouth as well as the throat and lungs. If you are a smoker, it’s important to let your dentist know what type of product you consume so they can screen you more frequently for cancer risks and oral health diseases.
The post What You Don’t Want To Read, But Need To See, About Smoking And Your Mouth appeared first on Fort Worth Dentist | 7th Street District | H. Peter Ku, D.D.S. PA.
What You Don’t Want To Read, But Need To See, About Smoking And Your Mouth posted first on http://dentistfortworth.blogspot.com

