There’s a load of anecdotal data about teens and young adults (TYAs) and their always-on relationship with mobile phones and social networks. There are also hundreds of stories written in both mass media outlets and professional journals on the topic of TYAs and mental health: especially relative to depression and suicidality.
In a breakthrough study, Hopelab and the Well Being Trust have sponsored the first deep-dive into the many dimensions of young people, their relationship with social media, and depression in Digital Health Practices, Social Media Use, and Mental Well-Being Among Teens and Young Adults in the U.S.,
The report was co-written by Victoria Rideout and Susannah Fox, two names Health Populi readers should know. Rideout is the go-to expert on media and health, with a special interest in children and media. Fox is the go-to person on the role of the internet in healthcare, and particularly the opportunity for digital tools to enable peer-to-peer support.
The study is based on a survey of over 1,300 U.S. teens and young adults, ages 14 to 22, polled in February and March 2018.
As I write up my read on the survey results, I will use the acronym “TYAs” alternating with the phrase “young adults,” to refer to the cohort of 14-22 year old’s surveyed in this study.
The top-line findings alone provide an important baseline profile of TYAs’ use of the internet for health never before described. Nearly 9 in 10 young adults have gone online to seek health information. Two-thirds have used a mobile app related to health. And, 61% of TYAs have read or watched someone else’s health story online.
4 in 10 young people have looked for people with similar concerns online — which is the real power of “social” in “social media.”
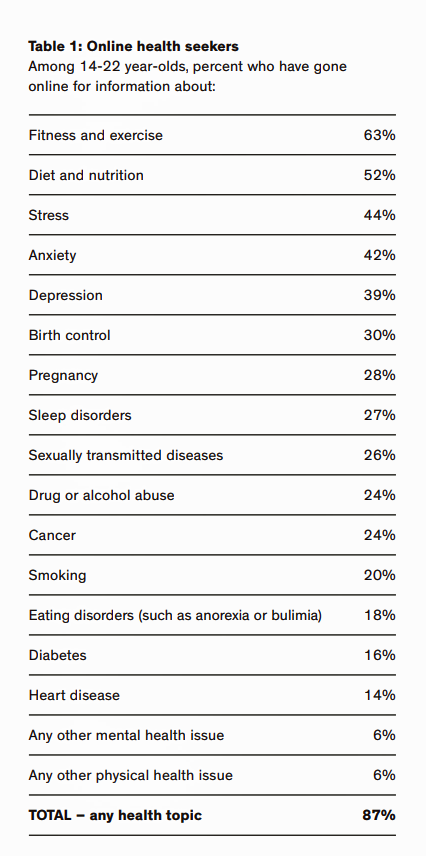
Nearly two-thirds of young people seek health information about fitness and exercise, one-half for diet and nutrition, 44% on stress, 42% on anxiety, and 39% on depression. Over 1 in 4 TYAs seek information on sexual health — birth control, pregnancy, and sexually transmitted disease.
And one-fourth seek information on sleep disorders and cancer. Table 1 lists the various search themes conducted by TYAs.
What’s fascinating about the top several responses is that they match the health topics most often sought by most U.S. adults, found in other studies.
The most popular mobile health apps young people use deal with fitness (42%), nutrition (26%), sleep (20%), period/menstruation (20%), and meditation/mindfulness (11%), closely followed by stress reduction (9%).
While a majority of both young women and young men look for health information online, use a mobile health app, and have watched or listened to someone else’s health experience online, at the margin, more females do so than males.
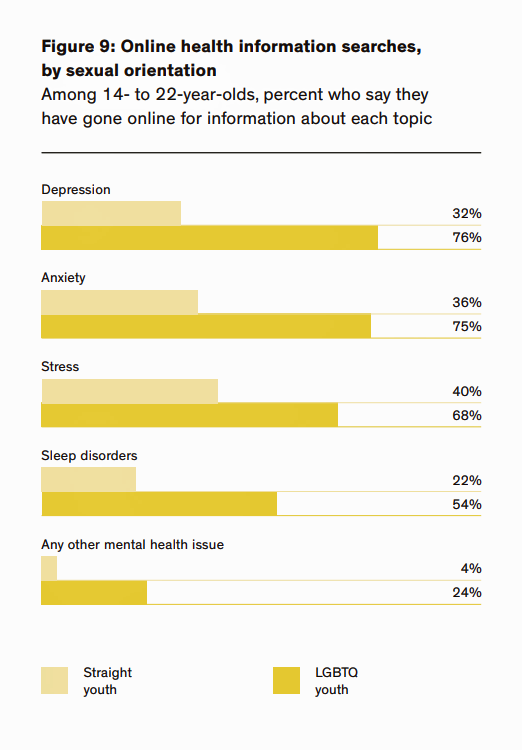 There’s another important difference in use of online health resources regarding TYAs who identify as LGBTQ versus straight youth: many more LGBTQ young
There’s another important difference in use of online health resources regarding TYAs who identify as LGBTQ versus straight youth: many more LGBTQ young
adults seek health resources online than straight young adults, for information on depression (76% vs. 32%), anxiety (75% vs. 36%), stress (68% vs. 40%), and sleep disorders (54% compared with 22%). The second yellow bar graph shows these differences.
This segues into critically important findings on young people and mental well-being. While one-half of respondents reported no depressive symptoms, one-quarter of young adults said they had mild depressive symptoms, and 25% reported moderate-to-severe symptoms of depression.
Those young people reporting moderate-to-severe depressive symptoms also go online for health information more than peers who report no depressive symptoms: for any health topic, any mental health topic, or for knowledge about depression, stress or anxiety. Young people with greater depressive symptoms also use health related mobile apps more than TYAs without depressive symptoms, for all health topics polled in the study – for both general health and behavioral health applications.
 Finally, young people with symptoms of depression also seek peer-to-peer health advice more frequently than TYAs with no depressive symptoms.
Finally, young people with symptoms of depression also seek peer-to-peer health advice more frequently than TYAs with no depressive symptoms.
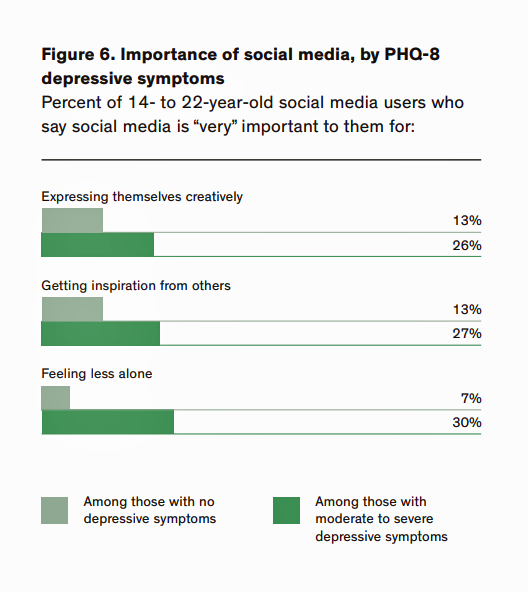
The third bar graph (in green) may be surprising. While social media use has gotten a rap for taking young people to the “dark side,” this study finds that more young people with depressive symptoms tend to find social media important for self-expression and creativity (by a factor of 2:1), feeling inspired by other people (again, by a factor of 2:1), and feeling “less alone,” for 30% of TYAs with depressive symptoms vs. only 7% of those with no signs of depression.
The authors offer recommendations for “the rest of us” to consider in meeting young peoples’ mental well-being challenges vis-a-vis digital tech and social networks:
- How can we develop better, more effective and empathetic digital tech that inspires, resonates, and addresses young peoples’ health concerns and needs?
- How can we further support and encourage young peoples’ peer-to-peer health experiences?
- How can we help young people “curate” and “titrate” the best digital health resources that can support positive relationships with themselves, others, and the health/care system?
- How can we support all young people, regardless of their sexual orientation, in nurturing positive relationships with themselves, their peers, their families, and communities-at-large?
Health Populi’s Hot Points: We refer to younger people as “digital natives,” having grown up with the online world as, well, just part of the everyday life-flow. It is not surprising, then, that young people use the internet, social networks, and apps for health as they do for all aspects of daily living.
What’s striking, however, is how natural it has become for young people to “hack” their way to wellness when they can, especially in seeking other “people like me,” dealing with stuff I’m dealing with. This is particularly important, the data demonstrates, for young people who may be made to feel like an “other” — those identifying as LGBTQ. We know the data that, shamefully, shows that people who are gay have a higher incidence of suicidality, of depression and anxiety, as well as less access to health care services. The fact that some younger people who identify as LGBTQ have found ways to leverage technology to feel inspired, to feel connected, and to find a safe place for expression is encouraging…and a place to begin to understand how to meet people where they “are.”
Several quotes jumped off the report page to me. I include three here that particularly resonated with me.
![]()
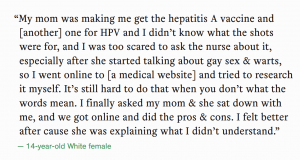
‘
In the case of teens and young adults, they are massively online, and that’s the reality for health information seeking, partnering, friending, finding a ride, joining a club, applying to college, finding a roommate….and just living.
This report gives us a place to start to wrestle with the demons of mental well-being for young people, knowing that digital tech and social networks will be part of the prescription for helping to make health and healthcare better with, and not just “for,” teens and young adults.
Thanks to Hopelab and the Well Being Trust for sponsoring this important research.
The post A Breakthrough, Sobering Report on Teens and Young Adults, Digital Health and Social Media Use: Implications for Mental Health appeared first on HealthPopuli.com.
A Breakthrough, Sobering Report on Teens and Young Adults, Digital Health and Social Media Use: Implications for Mental Health posted first on http://dentistfortworth.blogspot.com

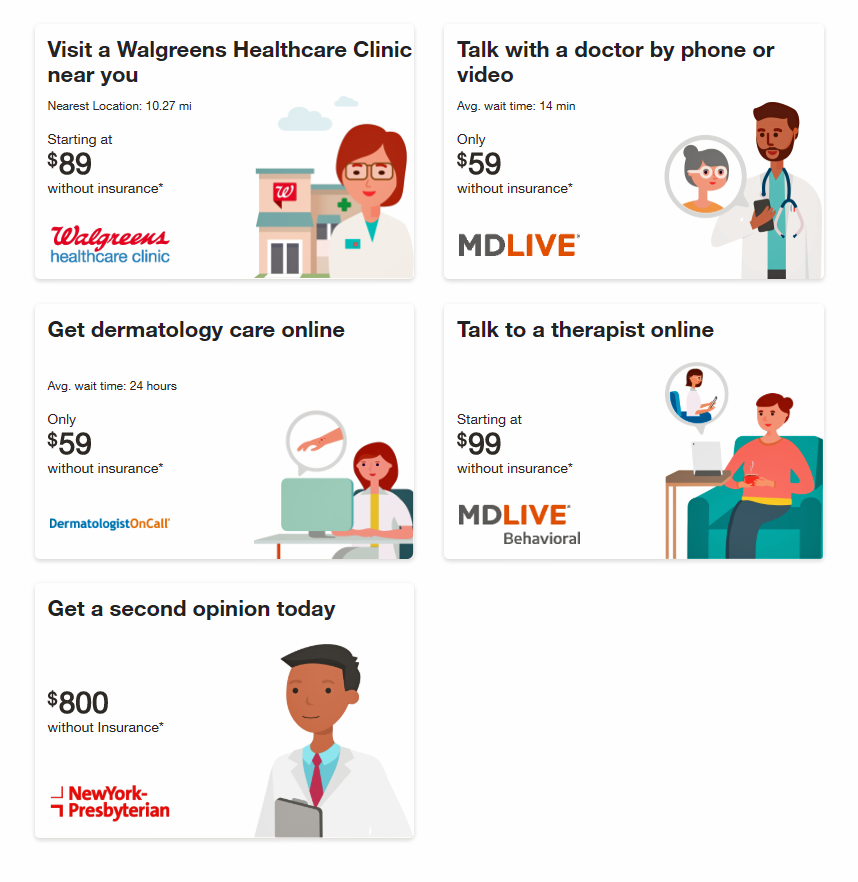 The latest news from Walgreens is their launch of
The latest news from Walgreens is their launch of  Media coverage of this story couches the Find Care Now program in terms of the Amazon’ing of health care. But that diminishes what Walgreens has already built in terms of institutional memory and health/care ethos. The company has over 78,000 healthcare service providers, including pharmacists, pharmacy technicians, nurse practitioners and other health capital. It’s a brand that 8 million consumers interact with every day, online and in any one of over 8,100 bricks-and-mortar stores located within a few miles of most Americans in all 50 U.S. states.
Media coverage of this story couches the Find Care Now program in terms of the Amazon’ing of health care. But that diminishes what Walgreens has already built in terms of institutional memory and health/care ethos. The company has over 78,000 healthcare service providers, including pharmacists, pharmacy technicians, nurse practitioners and other health capital. It’s a brand that 8 million consumers interact with every day, online and in any one of over 8,100 bricks-and-mortar stores located within a few miles of most Americans in all 50 U.S. states.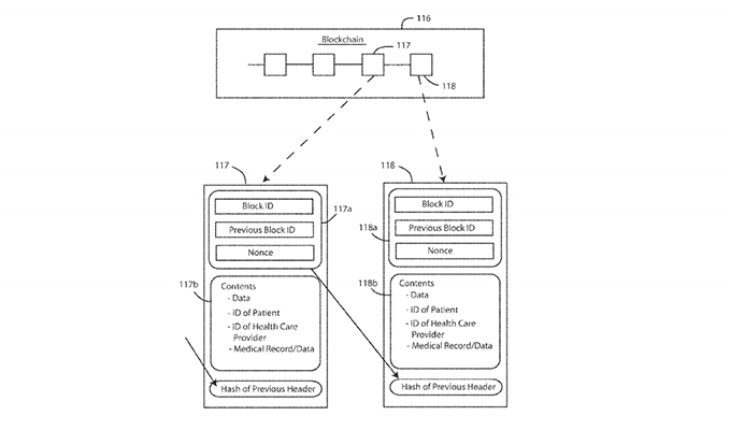 Another key announcement was Walmart’s relationship with Microsoft for cloud computing via MSFT’s Azure. This competes with the Amazon Web Service’s cloud business which has a lot of healthcare data in there already across the healthcare ecosystem’s segments. But don’t count out Microsoft, which has a long history serving both legacy healthcare (providers, plans, pharma) and new-new digital health programs and companies around the world. There are deep and serious healthcare chops here from which Walmart can benefit.
Another key announcement was Walmart’s relationship with Microsoft for cloud computing via MSFT’s Azure. This competes with the Amazon Web Service’s cloud business which has a lot of healthcare data in there already across the healthcare ecosystem’s segments. But don’t count out Microsoft, which has a long history serving both legacy healthcare (providers, plans, pharma) and new-new digital health programs and companies around the world. There are deep and serious healthcare chops here from which Walmart can benefit.
 Only 17% of Americans over 50 years of age shopped for groceries online by mid-2018. But older people in the U.S. have underlying demands and needs that could nudge them to do online grocery shopping, unearthed in
Only 17% of Americans over 50 years of age shopped for groceries online by mid-2018. But older people in the U.S. have underlying demands and needs that could nudge them to do online grocery shopping, unearthed in 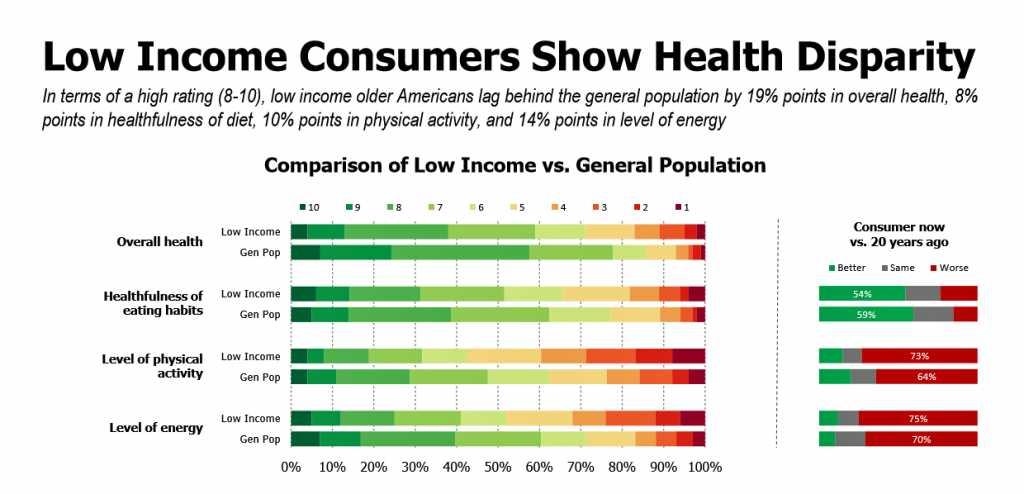 Lower income Americans over 50 face even more challenges when shopping for food in general,
Lower income Americans over 50 face even more challenges when shopping for food in general, 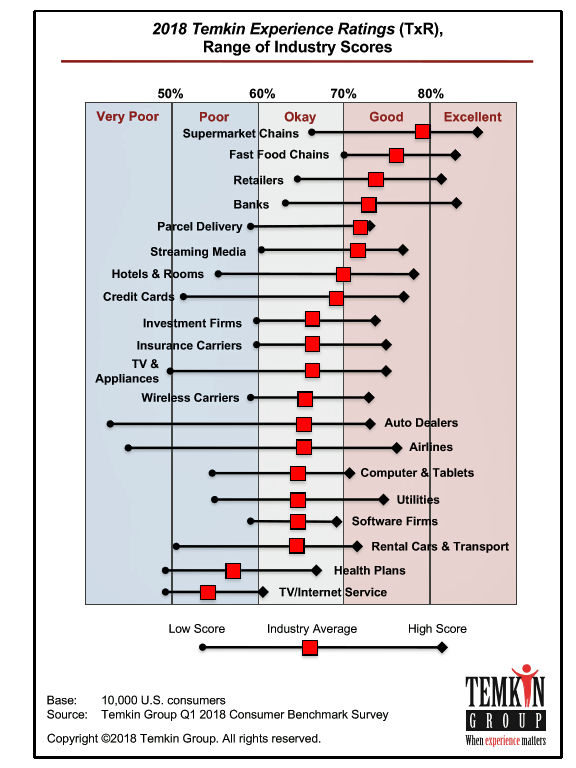 Health Populi’s Hot Points: Grocery stores ranked highest in the 2018 Temkin Experience Ratings. Look carefully at the chart here from Temkin’s latest consumer poll, and see where health plans lie in consumer experience: dead last with TV and internet service providers (THINK: Comcast, Verizon, et al).
Health Populi’s Hot Points: Grocery stores ranked highest in the 2018 Temkin Experience Ratings. Look carefully at the chart here from Temkin’s latest consumer poll, and see where health plans lie in consumer experience: dead last with TV and internet service providers (THINK: Comcast, Verizon, et al).

 Health Populi’s Hot Points: On a recent walk through Manhattan, I happened upon this ad in a bus stop kiosk promoting the wearable fitness tech products sold at Macy’s. “Macy’s?” you ask. Wearable tech is an important category these days in department stores, with discount retailers like Target and Walmart, at electronics outlets like Best Buy and, of course, via Amazon’s wearable tech ma
Health Populi’s Hot Points: On a recent walk through Manhattan, I happened upon this ad in a bus stop kiosk promoting the wearable fitness tech products sold at Macy’s. “Macy’s?” you ask. Wearable tech is an important category these days in department stores, with discount retailers like Target and Walmart, at electronics outlets like Best Buy and, of course, via Amazon’s wearable tech ma

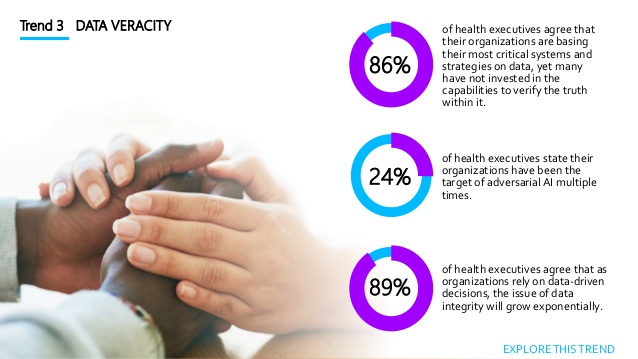 Data veracity speaks to the data “speaking the truth.” The root of the word “veracity” is “ver,” as in the Spanish “verdad,” or the Greek, “In vino veritas.” Veracity here confronts data’s potential to be noisy, biased, or otherwise “abnormal.” One in 4 health care executives say they’ve been the target of AI bad behaviors like falsified location data and bot fraud more than once. Unsurprisingly, then, 3 in 4 health execs aren’t ready to deal with the “impending waves” of corrupted insights as faked data or faulty algorithms touch healthcare databases.
Data veracity speaks to the data “speaking the truth.” The root of the word “veracity” is “ver,” as in the Spanish “verdad,” or the Greek, “In vino veritas.” Veracity here confronts data’s potential to be noisy, biased, or otherwise “abnormal.” One in 4 health care executives say they’ve been the target of AI bad behaviors like falsified location data and bot fraud more than once. Unsurprisingly, then, 3 in 4 health execs aren’t ready to deal with the “impending waves” of corrupted insights as faked data or faulty algorithms touch healthcare databases.