In the health care world, it is now commonly accepted that genes contribute less than half of the influence on peoples’ health status. Other issues play starring roles in overall well-being, including environmental factors, health care services, and social determinants of health (SDOH).
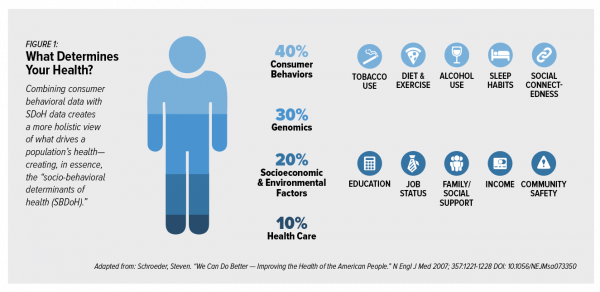 These inputs include education, personal economics (like job security and financial stability), physical built environments (think: transportation access, safe and healthy housing), food and nutrition, and access to health care.
These inputs include education, personal economics (like job security and financial stability), physical built environments (think: transportation access, safe and healthy housing), food and nutrition, and access to health care.
At HIMSS17, I gave a talk in a big room about how technology can scale SDOH; we had standing room only, which is not a brag — just a fact of the pent-up demand for this topic just two years ago. This year at HIMSS19, we can take part in at least two dozen education sessions preaching and teaching the centrality of SDOH in patient care and revenue cycle management, and exhibitors who are bringing SDOH data elements and analytics into the electronic health record.
 One of those sessions will be a panel in which I’ll participate on Tuesday 12 February hosted by NextGate and convened by John Lynn on this topic. Our theme is Embracing Social Determinants (SDoH) for Highly-Integrated, Coordinated Care. My compatriots will be Lygeia Ricciardi, Chief Transformation Officer at Carium; Minakshi Tikoo, CEO of REAPm; and, Daniel Cidon, CTO of NextGate Solutions. We’ll be brainstorming the current state of SDoH adoption in health care delivery, what’s preventing further adoption, and what we would do with a magic wand to promote a full health care ecosystem embrace of SDoH.
One of those sessions will be a panel in which I’ll participate on Tuesday 12 February hosted by NextGate and convened by John Lynn on this topic. Our theme is Embracing Social Determinants (SDoH) for Highly-Integrated, Coordinated Care. My compatriots will be Lygeia Ricciardi, Chief Transformation Officer at Carium; Minakshi Tikoo, CEO of REAPm; and, Daniel Cidon, CTO of NextGate Solutions. We’ll be brainstorming the current state of SDoH adoption in health care delivery, what’s preventing further adoption, and what we would do with a magic wand to promote a full health care ecosystem embrace of SDoH.
That magic wand would wish for clinicians to ask patients and caregivers about their lives, divining SDoH challenges to include in the full profile of the person in her/his EHR. That wand has begun to initiate its magic in the physician community, based on a wonderful essay in JAMA published 20 December 2018 titled, Social Determinants of Health in the Digital Age: Determining the Source Code for Nurture. The authors, doctors all, from Stanford, U-Colorado, and Yale med schools, note that, “Data from social media has the potential to improve understanding of the social determinants of health in a deeper way than prior data sources have ever allowed.” They explain that bring social network-generated data into the SDoH data ecosystem “could lead to novel, more nuanced understanding of social and behavioral variables that account for the interplay of the individual and the network in relation to health outcomes,” transforming the traditionally-held SDoH elements I listed above.
A person’s number of online friends, and more complex social biomarkers like timing of messages, frequency, and patterns of posts can help paint a profile of a person’s whole life.
This noble vision is accompanied by risks and challenges: namely, legal and ethical frameworks that are important guardrails to ensure health citizens’ rights. What options do people have to opt out of sharing their personal/social data? What does “de-identification” mean in this scenario? Does the U.S. need a new-and-improved HIPAA or more over-arching new national privacy law like a USGDPR?
 Waystar, a company that supports revenue cycle management in health care, published a survey report on Consumer perspectives on how social determinants impact clinical experience. The bottom line of this fascinating look into consumers’ views on health and SDoH is that people-as-patients well understand their health and social risks that threaten it. The data tell this story: two-thirds of patients who self-report their health as excellent have low to no SDoH risk. Conversely, nearly one-half of patients who self-report poor-health are at high SDoH risk.
Waystar, a company that supports revenue cycle management in health care, published a survey report on Consumer perspectives on how social determinants impact clinical experience. The bottom line of this fascinating look into consumers’ views on health and SDoH is that people-as-patients well understand their health and social risks that threaten it. The data tell this story: two-thirds of patients who self-report their health as excellent have low to no SDoH risk. Conversely, nearly one-half of patients who self-report poor-health are at high SDoH risk.
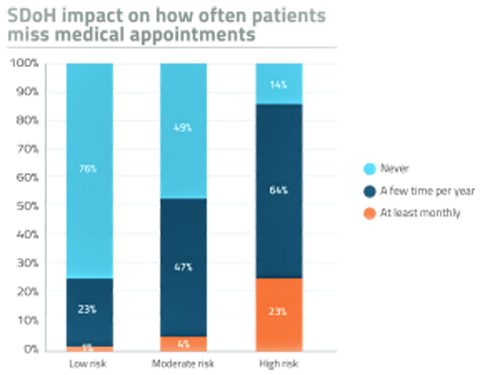
Check out this chart from the Waystar study, showing that nearly one in four patients at high-risk miss medical appointments at least once a month, and two-thirds miss appointments a few times a year. Access to health care services is a core social determinant for health, and there are many reasons people can miss appointments. One is transportation, which is getting a lot of play at HIMSS19. I noted walking into the Convention Center on Monday several big ad placements from Lyft, found on large cement pillars outside of the building, and inside on glass doors separating one section of the Center from another.

Patients most-trust their clinicians, physicians and nurses, as safe places in which to have an honest SDoH discussion, compared with a health insurance representative. But age is a factor in these conversations, where younger people are more comfortable talking about SDoHs with clinicians than older people. Yet it’s older people who are more at-risk for SD0H challenges. Ironically older people are more receptive to receiving SDoH support, compared with younger people who are more resistant, Waystar found.
Health Populi’s Hot Points: This photo I snapped of one of the Lyft promotions states that, “90% of seniors say access to Lyft improves their quality of life.” Note the AARP banner logo at the bottom of the poster, lending a brand trust “halo” to the ad that could resonate with millions of older Americans who belong to the Association.
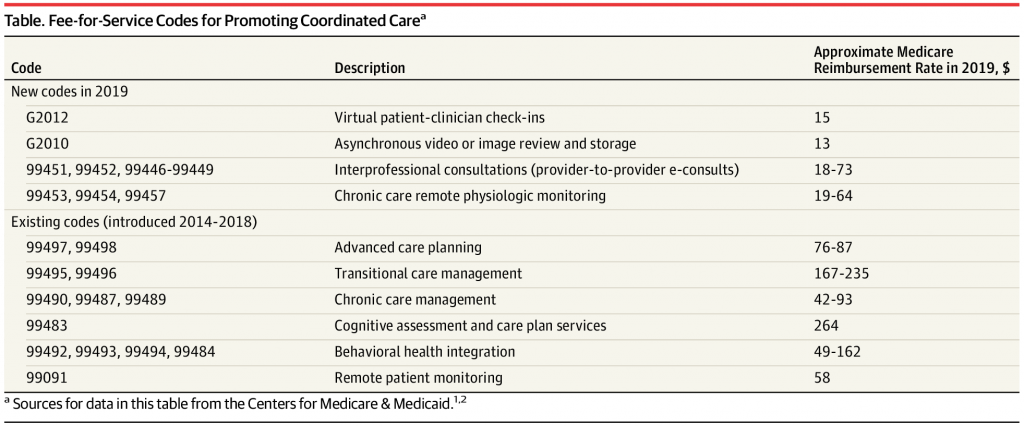 To mitigate SDoH risks for older Americans, Medicare has begun to pay for services that promote coordinated care. The 2019 Physician Fee Schedule from the Centers for Medicare & Medicaid Services (CMS) published new billing codes for services that allow clinicians to prescribe asynchronous telehealth services, e-consults between clinicians to consult on a patient case, and virtual check-ins for patients and their doctors. This could improve continuity of care between transitions from hospital to rehab to home, chronic care management, behavioral health, and other fragmented health care services.
To mitigate SDoH risks for older Americans, Medicare has begun to pay for services that promote coordinated care. The 2019 Physician Fee Schedule from the Centers for Medicare & Medicaid Services (CMS) published new billing codes for services that allow clinicians to prescribe asynchronous telehealth services, e-consults between clinicians to consult on a patient case, and virtual check-ins for patients and their doctors. This could improve continuity of care between transitions from hospital to rehab to home, chronic care management, behavioral health, and other fragmented health care services.
Payment is prophecy for health care adoption in a fee-for-service environment. As health care delivery in the U.S. continues to migrate, ever slowly, toward value-based payment regimes, paying for services that de-fragment health care for those at most risk will help both clinicians and patients toward better care at a lower cost.
A paper from Acxiom on using data to deliver better patient-driven experiences and outcomes concludes with a quote from Clark Wooten who leads the company’s insurance and healthcare practices: “There is a cultural shift required to achieve…transformation. The technology is there; it’s the processed and people that need to align with that technology to realize its true value.”
CMS’s service codes, which will enable payment to clinicians for prescribing coordinated care services, will help to nudge that alignment.
The post Health Is Social – The Social Determinants of Health at HIMSS19 appeared first on HealthPopuli.com.
Health Is Social – The Social Determinants of Health at HIMSS19 posted first on http://dentistfortworth.blogspot.com
No comments:
Post a Comment