“The promise of AI is undeniable…could AI help clinicians deliver better and more humanistic care?” This question is asked and answered in a JAMA viewpoint published January 1/8 2019 titled, Humanizing Artificial Intelligence.
This theme motivated a conversation held over a dinner convened by Philips hosted by Frans Van Houten this week at HIMSS19.
 To provide context Geoff Colvin, Fortune‘s Senior Editor, first talked about taking friction out of industries, as Lyft and Uber have done in the transport sector. “Taking friction out of industries challenges and changes business models,” Georff noted. With Uber’s IPO valuation approaching $100 billion, I’d say that’s some business model.
To provide context Geoff Colvin, Fortune‘s Senior Editor, first talked about taking friction out of industries, as Lyft and Uber have done in the transport sector. “Taking friction out of industries challenges and changes business models,” Georff noted. With Uber’s IPO valuation approaching $100 billion, I’d say that’s some business model.
This is a phenomenon that has impact across all industries, where business model innovation is now a core competence for all sectors, Geoff said.
In healthcare it’s difficult to take friction out of such a complex and highly regulated industry. But with big problems come big opportunities.
Artificial intelligence, AI, is a huge theme at HIMSS19. It also has the potential of being an enormous boon to humanity, Geoff imagined. AI is the type of tool that economists (my own professional guild) refer to as a “general purpose technology” because it crosses all industries. THINK: electricity and the open Internet, for examples.
Organizations today are struggling with how to get a grip on AI and apply the tool in their businesses: where and how much to invest? What is the business case for AI in our enterprise right now? they ask.
Geoff said there’s one core truth to consider: that humans will be economically valuable to the extent they can use deep human interaction.
This is why AI may have the biggest impact on health care compared with other industries, he posited.
The human side of the AI/human interface is so valuable, particularly in health care: evidence shows that we have better health outcomes if the caregiver relationship is better, stronger, and resilient.
Now, consider the root problems that the Quadruple Aim addresses: drive health outcomes, enhance the health experience for both patient and provider to prevent burnout, and lower per capita medical costs.
In health/care, the real business we are in is a relationship business.
 Geoff introduced Philips’ CEO, saying, “Frans made Philips a health care company.”
Geoff introduced Philips’ CEO, saying, “Frans made Philips a health care company.”
In his introductory remarks, Frans called out that health care is unaffordable. The system will face growing demands based on lifestyle-driven diseases and the natural course aging. Eventually, he said, the medical bill needs to be contained. This is a global challenge for health systems around the world, although a particularly unsustainable challenge for volume-driven fee-for-service payment in the U.S.
Combine that demand side on the consumer/patient side with the fact that pressures in health care delivery organizations are creating dissatisfaction among health care workers, a Bain study recently observed looking at the “front line of health care.”
That’s one leg of the 4-part Quadruple Aim stool: to enhance health care experience for both patients and providers. A burned-out clinician is not an ingredient for bolstering a resilient, high performing health system.
How? Frans asked.
He responded to his question: “Innovation must be purposeful for clients.” Philips invests $1.8 billion on R&D, using the lens of the Quadruple Aim to measure innovation by that definition. If the R&D spend on a particular area doesn’t score on the Quad-Aim metrics, “we are doing something wrong,” Frans believes. “We must embrace courage while avoiding unproductive tangents.”
Focusing in on AI, Frans described, “We are in a Valhalla of innovation where there are false starts…we’re on a learning curve regarding AI. We [prefer to] talk about ‘adaptive’ not ‘artificial’ intelligence.”
For new business models, we need to engage in “creative and brave conversations” with payors, providers and patients, Frans believes. That’s part of developing deep human interactions with stakeholders in health care. Getting into these discussions can yield rich insights: for example, better understanding and empathizing with the role of the patient-as-consumer-as-payer in the context of the hospital CFO’s challenges with revenue cycle management and collections, with social work’s concerns about continuity of care once the patient leaves the hospital, could result in a creative solution to provide rich and well-designed information at the time of discharge that surrounds the patient with a feeling of empowerment and engagement adapted for them.
Once home, if the patient engages in effective self-care, she can prevent a readmission which then can help the hospital conserve costs. “Saving 30% of costs would create the oxygen to do really interesting things,” Frans explained.
In this moment of AI fear and trepidation, Frans explained, “AI is often seen as an implied threat…but it doesn’t have to be a massive mystical threat….It won’t profoundly impact ‘tomorrow’ but is a reason to optimize operations today.”
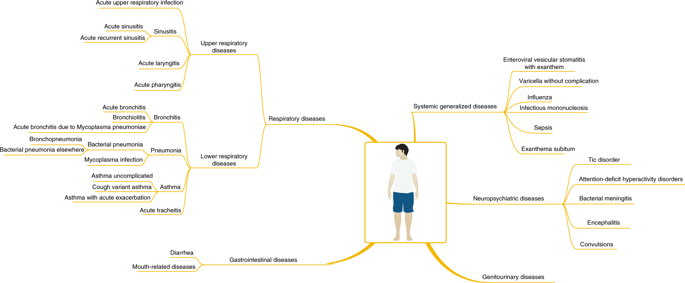 Frans pointed us to a just-published article in Nature Medicine on using AI for more effectively diagnosing childhood diseases. The study mashed up 101.6 million data points from 1,362,559 pediatric patient visits to a health system. Various pediatric conditions assessed in the study are shown in this diagram from the study. The data model proved accurate compared with pediatricians diagnosing common childhood conditions.
Frans pointed us to a just-published article in Nature Medicine on using AI for more effectively diagnosing childhood diseases. The study mashed up 101.6 million data points from 1,362,559 pediatric patient visits to a health system. Various pediatric conditions assessed in the study are shown in this diagram from the study. The data model proved accurate compared with pediatricians diagnosing common childhood conditions.
AI won’t replace those pediatricians, but can enhance their diagnostic toolbox and also help scale care to under-served communities.
At the end of the day, the JAMA column on humanizing artificial intelligence concludes that, “Humans in need want the best of what science and medicine have to offer…Bettering the ability of physicians to truly care for and express caring is the challenge for colleagues in computer science and medical informatics….is it possible to invent and discover applications that can enhance the human abilities in clinicians to better engage in caring for hte patient?”
This was the intention of the Philips team in convening us to ponder the theme of leveraging 21st century technology to reinvent health care at HIMSS19. At this year’s conference, AI has been a major theme discussed in both education sessions and on the exhibit floor. We would be wise to embrace this humanistic approach to AI (whether we consider the “a” as artificial, adaptive, augmented, awesome or alarming). As consumers learn more about the promise of AI, they will also look to organizations to utilize AI in the context of corporate social responsibility and fair play.
The post Deep Human Interactions: The Antidote To More AI In Health Care – Learning From Philips’ CEO At HIMSS19 appeared first on HealthPopuli.com.
Deep Human Interactions: The Antidote To More AI In Health Care – Learning From Philips’ CEO At HIMSS19 posted first on http://dentistfortworth.blogspot.com
No comments:
Post a Comment