“The Fourth Industrial Age,” Dr. Abraham Verghese writes, “has great potential to help, but also to harm, to exaggerate the profound gap that already exists between those who have much and those who have less each passing year.”
Dr. Verghese asserts this in his forward to Deep Medicine, Dr. Eric Topol’s latest work which explores the promise of artificial intelligence (AI), Big Data, and robotics — three legs of the Fourth Industrial Age stool.
[If you don’t know the work of Dr. Verghese, and since you’re reading the Health Populi blog, you must get to know Dr. V now. Your first dip into his wisdom should be “A Doctor’s Touch,” his TED talk from 2011 with over 1.5 million views. You will thank me for pointing you to this pearl. You will want to know more. But before diving deeply, let’s return to the main vein of this post, Dr. T’s latest].
We want our physicians to know us, deeply indeed, through all of our “omes:” genome, proteome, metabolome, transcriptome, and so on, Dr. V observes. We want our physicians to give us time and attention, “to acknowledge the locus of disease on our body and not on a biopsy or an image or a report,” he continues.
Ultimately, we want our doctors to know, “what we live for and would die for,” Dr. V concludes his forward.
Thus begins the promise of Deep Medicine, and how AI can make healthcare human again, via Dr. Topol’s tagline to the title.
This book picks up where The Patient Will See You Now and The Creative Destruction of Medicine leave off…on the future of medicine, versus what’s led up to where we are now. In the first chapter introducing the concept of “deep medicine,” Dr. Topol starts with the
 He follows up the promise of AI in chapter two, discussing the deep economic mess American health care is in. This is familiar territory here in Health Populi where we cover every nook and cranny of dismal U.S. health economics, and hopeful green shoots for making health care more cost-effective, high quality, engaging and even enchanting-by-design. “Shallow Medicine” is the theme of this discussion, which includes the word cloud shown here describing Americans’ views on doctors in 2017, published in a JAMA Surgery article called, “Patient Perceptions About Their Physician in 2 Words: The Good, the Bad, and the Ugly.”
He follows up the promise of AI in chapter two, discussing the deep economic mess American health care is in. This is familiar territory here in Health Populi where we cover every nook and cranny of dismal U.S. health economics, and hopeful green shoots for making health care more cost-effective, high quality, engaging and even enchanting-by-design. “Shallow Medicine” is the theme of this discussion, which includes the word cloud shown here describing Americans’ views on doctors in 2017, published in a JAMA Surgery article called, “Patient Perceptions About Their Physician in 2 Words: The Good, the Bad, and the Ugly.”
The U.S. spends too much money for too little ROI on that spending, from hospital care and dental services to prescription drugs and what ultimately illustrates wasted life and potential in American society: maternal, infant and child mortality, which is by far the worst outcome in a developed nation and as bad as some much poorer countries experience.
Shallow calls for Going Deep for medical diagnosis, Dr. Topol argues, talking about the opportunities afforded by looking at a cluster of symptoms, second (or more) opinions, crowdsourcing diagnoses, and leveraging citizen science: the role of engaged lay people who share the details of their illnesses and pay-it-forward through that sharing — for peer patients today, and future patients.
Dr. Topol then teaches us about the Skinny on Deep Learning, making sure we understand that getting labels and “ground truths” right is critical for building useful algorithms. But wait — what’s an algorithm, anyway? It’s more than “if this, then that,” Dr. T. warns. He quotes Massimo Mazzotti of UC Berkeley, who calls out that “algorithm” means a program running on a physical machine, as well as its effects on other systems. This is obviously important as doctors grow to count on AI in medicine with a systems perspective on human health.
 Furthermore, Dr. T. refers us to Yuval Noah Harari whose book Homo Deus is groundbreaking (and a must-read for Health Populi readers, too). “‘Algorithm’ is arguably the single most important concept in our world. If we want to understand our life and our future, we should make every effort to understand what an algorithm is, and how algorithms are connected with emotions….99 percent of our decisions…are made by the highly refined algorithms we call sensations, emotions and desires,” Harari wrote in his book. He’s very concerned about faith in algorithms’ power, Dr. T observes, noting Harari says that faith is “dataism.”
Furthermore, Dr. T. refers us to Yuval Noah Harari whose book Homo Deus is groundbreaking (and a must-read for Health Populi readers, too). “‘Algorithm’ is arguably the single most important concept in our world. If we want to understand our life and our future, we should make every effort to understand what an algorithm is, and how algorithms are connected with emotions….99 percent of our decisions…are made by the highly refined algorithms we call sensations, emotions and desires,” Harari wrote in his book. He’s very concerned about faith in algorithms’ power, Dr. T observes, noting Harari says that faith is “dataism.”
With this caveat in mind, Dr. T explains that algorithms lie on a continuum from human guided to entirely machine guided. These latter algorithms are the deep learning ones, deep neural networks (DNNs). Four converging forces underlie DNNs:
- Big Data sets
- Dedicated graphic processing units (GPUs) which are the founding for speedy computations
- Cloud computing and the ability to store massive amounts of data, and
- Open-source algorithms.
DNNs have already been adopted in gaming, images (useful for image recognition for biometrics, for example), voice/speech/translation, and autonomous cars. Ironically, Dr T points out that “neural networks” really aren’t all that “neural.” Brains really don’t work like machines.
Deep learning AI complements human learning, Dr. T asserts. There’s bias in algorithms, and bias in human thinking, too, explored in the chapter “Deep Liabilities.” We know bias is, “baked into the system,” Dr. T admits, because patients in clinical trials are rarely generalizable to the overall population. The inequities have medical implications, Harari wrote in Homo Deus: “twentieth century medicine aimed to heal the sick, but twenty-first century medicine is increasingly aiming to upgrade the healthy.” There’s an AI-fueled gap between have’s and have not’s, with AI biases often adversely impacting the most vulnerable people in society.
 With this further caveat in mind, recognizing that U.S. public policy in current form protects neither the vulnerable nor the hackable, Dr. T talks about the promise of AI to enhance doctors’ ability to diagnose conditions “with patterns” and without patterns, along with detecting and supporting patients’ mental health. AI also supports health system management (like preventing readmissions or predicting staff requirements over a time period), discovering cures, informing nutrition based on N’s of 1’s, and providing care to people who may live in rural or under-served areas.
With this further caveat in mind, recognizing that U.S. public policy in current form protects neither the vulnerable nor the hackable, Dr. T talks about the promise of AI to enhance doctors’ ability to diagnose conditions “with patterns” and without patterns, along with detecting and supporting patients’ mental health. AI also supports health system management (like preventing readmissions or predicting staff requirements over a time period), discovering cures, informing nutrition based on N’s of 1’s, and providing care to people who may live in rural or under-served areas.
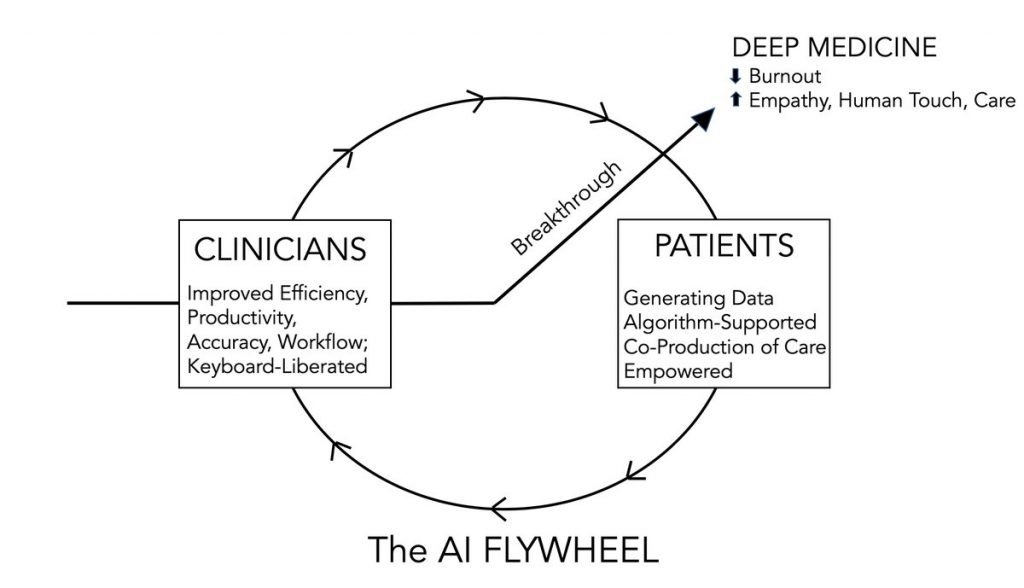
The promise is to drive Deep Empathy, the last chapter hopefully concludes. An introductory quote from Aldous Huxley (author of Brave New World) suggests where this section will go: “By these means we may hope to achieve not indeed a brave new world, no sort of perfectionist Utopia, but the more modest, and much more desirable objective — a genuinely human society.” Ideally, AI can give the clinician and the patient the gift of time, replacing the “scut work” and wasted work-flow with time to be human. Beyond time, people on both sides of the diagnosis and treatment process desire empathy. No machine will alleviate “suffering,” Dr T writes: this requires human-to-human bonding, time and trust.
The last page of the book takes on the book’s title, “Deep Medicine.” “We’re still in the earliest days of AI in medicine….long on computer algorithmic validation…but very short on real-world, clinical proof of effectiveness,” Dr T realizes. The triad of deep phenotyping, understanding a person’s many layered-data, deep learning, and deep empathy, could remedy the economic unsustainability in healthcare, he hypothesizes. That comes second to what’s even more important, bringing the book’s optimistic tagline full circle: “Presence. Empathy. Trust. Caring. Being Human.”
AI can help us restore the humanity between physicians and patients. At the end, Dr T says we must embrace the opportunity to do so.
 Health Populi’s Hot Points: In an essay last week in Brookings, Bob Kocher and Zeke Emanuel ask the question, “Will Robots Replace Doctors?” Kocher, a long-time venture capitalist who has funded many a health care innovator via the VC firm Venrock, and Dr. Emanuel, who heads the Department of Medical Ethics and Health Policy at the University of Pennsylvania along with being a venture partner at Oak HC/FT, speak to the public policy, economic, clinical and all-to-human challenge of AI bias. “Before we entrust our care to AI systems and ‘doctor robots,’ we must first commit to identifying bias in datasets and fixing them as much as possible. Furthermore, AI systems need to be evaluated not just on the accuracy of their recommendations, but also on whether they perpetuate or mitigate disparities in care and outcomes,” Kocher and Emanuel assert.
Health Populi’s Hot Points: In an essay last week in Brookings, Bob Kocher and Zeke Emanuel ask the question, “Will Robots Replace Doctors?” Kocher, a long-time venture capitalist who has funded many a health care innovator via the VC firm Venrock, and Dr. Emanuel, who heads the Department of Medical Ethics and Health Policy at the University of Pennsylvania along with being a venture partner at Oak HC/FT, speak to the public policy, economic, clinical and all-to-human challenge of AI bias. “Before we entrust our care to AI systems and ‘doctor robots,’ we must first commit to identifying bias in datasets and fixing them as much as possible. Furthermore, AI systems need to be evaluated not just on the accuracy of their recommendations, but also on whether they perpetuate or mitigate disparities in care and outcomes,” Kocher and Emanuel assert.
Addressing biased data sets and algorithms must be part of a new deal on health citizenship for Americans, who must also be in control of their personal health data and have a right to quality health care without regard to what state they live in, or whether they’re urban or rural communities. Bias delivered via AI is still bias, and would reinforce and exacerbate the health disparities that have marred American health care for decades and continue to do so.
My family and I are proponents of the Slow Food Movement. Founded in Italy, Slow Food is based on the idea that eating locally sourced food, cooked at home, by hand, shared and savored with other people bolsters health on all levels – physical, emotional, financial. That Eric Topol devoted an entire chapter to “Deep Diet” is further evidence that the good doctor gets more than digital health innovations: he also embraces the importance of food-as-medicine and nutrition as a social determinant of health, also one of grand disparities underlying health inequity in the U.S.
 One of our family mantras (in addition to Slow Food and the importance and gift of shared family mealtime) we ingrained in our daughter was to “go slow to go fast.” Festina lente, an Italian grandmother might quote Emperor Augustus or the Medici clan: “make haste, slowly.”
One of our family mantras (in addition to Slow Food and the importance and gift of shared family mealtime) we ingrained in our daughter was to “go slow to go fast.” Festina lente, an Italian grandmother might quote Emperor Augustus or the Medici clan: “make haste, slowly.”
With AI married to medicine, we can “go fast to go slow,” to the benefit of both patient and provider.
The post Can AI Make Healthcare Human Again? Dr. Topol Says “Yes” appeared first on HealthPopuli.com.
Can AI Make Healthcare Human Again? Dr. Topol Says “Yes” posted first on http://dentistfortworth.blogspot.com
No comments:
Post a Comment