
How long can people living in the U.S. expect to live? 78.6 years of age, if you were born in 2017.
That’s a decline of 0.1 year from 2016.
This decline especially impacted baby boys: their life expectancy fell to 76.1 years, while baby girls’ life expectancy stayed even at 81.1 years.
That’s the latest data on Mortality in the United States, 2017, soberly brought to you by the Centers for Disease Control and Prevention, part of the U.S. Department of Health and Human Services.
 Underneath these stark numbers are the specific causes of death: in 2017, more Americans died due to unintentional injuries, lower respiratory diseases, stroke, Alzheimer Disease, diabetes, influenza and pneumonia, and suicide, increasing in prevalence among the top ten causes of death in the U.S. On the upside, deaths fell due to cancer, and rates for heart and kidney disease stayed relatively even.
Underneath these stark numbers are the specific causes of death: in 2017, more Americans died due to unintentional injuries, lower respiratory diseases, stroke, Alzheimer Disease, diabetes, influenza and pneumonia, and suicide, increasing in prevalence among the top ten causes of death in the U.S. On the upside, deaths fell due to cancer, and rates for heart and kidney disease stayed relatively even.
There are three underlying stats that are particularly concerning in this report:
1. The rates of death for younger ages significantly grew between 2016 and 2017 in the age cohorts 25-34 and 35-44.
2. For infant deaths, unintentional injuries significantly rose over the year. There was also a marked increase in maternal complications.
3. Drug overdoses were the cause of over 70,000 U.S. deaths — related to the growing use of synthetic opioids.
 That’s due to the fact that the age-adjusted rate of drug overdose deaths with synthetic opioids (not methadone) increased by 45% between 2016 and 2017. This is shown in the third graphic, the line chart showing the hockey-stick growth of synthetic opioids since 2013.
That’s due to the fact that the age-adjusted rate of drug overdose deaths with synthetic opioids (not methadone) increased by 45% between 2016 and 2017. This is shown in the third graphic, the line chart showing the hockey-stick growth of synthetic opioids since 2013.
While there is obvious and important attention being paid to drug overdoses and the opioid crisis, and suicides among younger people, Americans should be mindful too of lack of significant progress dealing with mortality due to respiratory disease, stroke, Alzheimer’s, and the flu, along with infant deaths due to maternal complications and unintentional injuries.
Health Populi’s Hot Points: It’s a stark, sad reality that Americans are losing years of life that could be conserved. The nation spends more resources on healthcare than any country on Planet Earth, and the ultimate ROI should be life-years, and quality of those life-years.
 If you look at the map, you’re seeing states by the rate of drug overdoses in 2017. The higher-than-national-average rates are in dark blue. This is not to say there aren’t deaths due to overdose in the green-hued states. But this is one lens on one’s ZIP code being a risk factor for health, and in this case, death from overdosing.
If you look at the map, you’re seeing states by the rate of drug overdoses in 2017. The higher-than-national-average rates are in dark blue. This is not to say there aren’t deaths due to overdose in the green-hued states. But this is one lens on one’s ZIP code being a risk factor for health, and in this case, death from overdosing.
This challenge is but one of many that are, partly, addressable by getting real about social determinants. For these deaths of despair, job security and unemployment, social connections and loneliness, access to healthcare services (THINK: mental health, anxiety, depression, pain), and education are all pathways to socioeconomic status and social security (meant in the phrase as written, not as the U.S. Federal program of “Social Security”).
Three years ago here on Health Populi, I wrote about the deaths of despair, a phrase coined by Angus Deaton and Ann Case of Princeton. Then, I said,
“The authors note that the increase in midlife mortality is only partly understood. Increased availability of opioid prescription drugs, chronic pain (for which opioids are often prescribed), and the economic crisis which began in 2008 may all have contributed to an increase in overdoses, suicide, and increased liver disease associated with alcohol abuse.”
Three years later, there’s little national/Federal progress on resourcing the social determinants and personal/household economies that could help turnaround this public health challenge. (Most Americans didn’t feel a short-term sustained benefit from the recent tax reform legislation). While Congress and the President do chat about the opioid crisis, look for more action from the private sector and State Governors than Congress in 2019.
The post The Ultimate Health Outcome, Mortality, Is Rising in America appeared first on HealthPopuli.com.
The Ultimate Health Outcome, Mortality, Is Rising in America posted first on http://dentistfortworth.blogspot.com
 From culture to travel, food and drink to retail and beauty, health will be baked into consumer goods and experiences in 2019.
From culture to travel, food and drink to retail and beauty, health will be baked into consumer goods and experiences in 2019.
 Health Homekits Upgraded
Health Homekits Upgraded
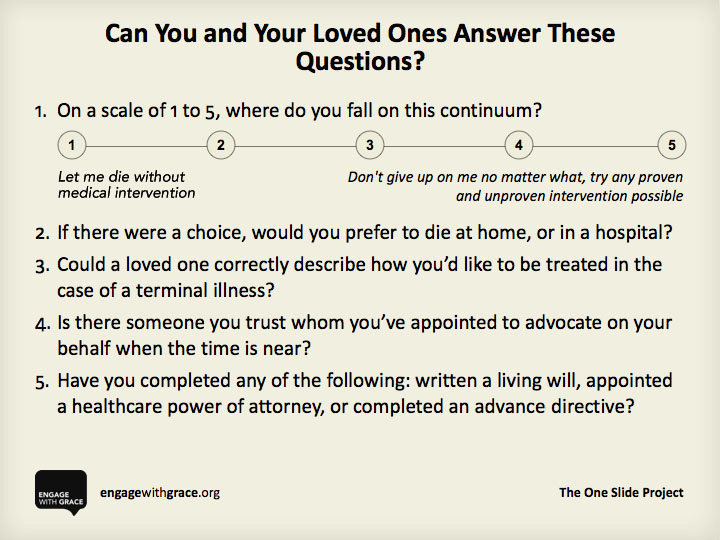 The right time to have that sensitive, considered, intimate dialogue is now, before that inevitable time comes for decision-making.
The right time to have that sensitive, considered, intimate dialogue is now, before that inevitable time comes for decision-making. Health Populi’s Hot Points: Every year, the day before Thanksgiving, I write this post on the Engage With Grace project and the opportunity to inspire an end-of-life conversation.
Health Populi’s Hot Points: Every year, the day before Thanksgiving, I write this post on the Engage With Grace project and the opportunity to inspire an end-of-life conversation.
 Consumers’ ranking an organization with a high societal ROI sounds like a “nice-to-have” rating. However, there’s a hard return-on-investment for companies that are top performers versus those who rank low. The second graphic shows that top performers compel a consumer to more likely say something positive about the organization; recommend the company as a good place to work; and, welcome the company expanding in the consumer’s community.
Consumers’ ranking an organization with a high societal ROI sounds like a “nice-to-have” rating. However, there’s a hard return-on-investment for companies that are top performers versus those who rank low. The second graphic shows that top performers compel a consumer to more likely say something positive about the organization; recommend the company as a good place to work; and, welcome the company expanding in the consumer’s community. Now we add data privacy to this mix — call it, “data well-being.” Because people are getting stressed about how their digital data — from retail receipts to gene and lab tests and wearable tech metrics — are being stored, stewarded and secured, and shared with third parties.
Now we add data privacy to this mix — call it, “data well-being.” Because people are getting stressed about how their digital data — from retail receipts to gene and lab tests and wearable tech metrics — are being stored, stewarded and secured, and shared with third parties.
 “Seeing is not believing” when it comes to people seeing health information on social networks. Four in five people seeking healthcare information online in social media are concerned about the accuracy of that information served up.
“Seeing is not believing” when it comes to people seeing health information on social networks. Four in five people seeking healthcare information online in social media are concerned about the accuracy of that information served up.
 American consumers are now viewing their phones an average of 52 times daily, with 39 percent of consumers believing they use their smartphones too much. In fact, 60 percent of 18 to 34-year-olds admit to smartphone overuse, the highest level of any age group. However, 63 percent of the respondents reported trying to limit their smartphone usage, roughly half succeeding in cutting back. Smartphones also are helping blur the lines between work and leisure with 70 percent of respondents using personal smartphones at least occasionally for after-hours work.
American consumers are now viewing their phones an average of 52 times daily, with 39 percent of consumers believing they use their smartphones too much. In fact, 60 percent of 18 to 34-year-olds admit to smartphone overuse, the highest level of any age group. However, 63 percent of the respondents reported trying to limit their smartphone usage, roughly half succeeding in cutting back. Smartphones also are helping blur the lines between work and leisure with 70 percent of respondents using personal smartphones at least occasionally for after-hours work. Now look at the second chart: this inventories consumers’ interests in using different technology devices for various online activities. You’ll see a lot of
Now look at the second chart: this inventories consumers’ interests in using different technology devices for various online activities. You’ll see a lot of  In 2018, one in five U.S. consumers used a fitness band, 14% a smartwatch, and 8% a virtual reality (VR) headset, shown in the third chart. Note the ten percent decline in use of fitness bands. This may be due to marginally more consumers using phones for tracking activities as the phones get better equipped with smarter sensors with more utility. Mic Locker, managing director in Deloitte’s Technology, Media & Telecommunications practice, noted a bright spot for wearables: that daily usage is growing for owners of fitness bands and smartwatches. So those who continue to use these devices are doing so more regularly.
In 2018, one in five U.S. consumers used a fitness band, 14% a smartwatch, and 8% a virtual reality (VR) headset, shown in the third chart. Note the ten percent decline in use of fitness bands. This may be due to marginally more consumers using phones for tracking activities as the phones get better equipped with smarter sensors with more utility. Mic Locker, managing director in Deloitte’s Technology, Media & Telecommunications practice, noted a bright spot for wearables: that daily usage is growing for owners of fitness bands and smartwatches. So those who continue to use these devices are doing so more regularly.
 Lisa is a mentor, both out-and-proudly and quietly, too. Long understanding and experiencing life as a woman in tech in Silicon Valley, well before media covered stories and #MeToo emerged, Lisa co-founded
Lisa is a mentor, both out-and-proudly and quietly, too. Long understanding and experiencing life as a woman in tech in Silicon Valley, well before media covered stories and #MeToo emerged, Lisa co-founded  In my own work forecasting healthcare, I do 1:3:5 year snapshots, with the 5 years more of a scenario planning exercise than a straight line projection given tech, social, political and wild card uncertainties across our health/care ecosystem.
In my own work forecasting healthcare, I do 1:3:5 year snapshots, with the 5 years more of a scenario planning exercise than a straight line projection given tech, social, political and wild card uncertainties across our health/care ecosystem. Diabetes is a family issue, and its prevalence is growing in America. November 14, 2018, is
Diabetes is a family issue, and its prevalence is growing in America. November 14, 2018, is  The rising costs of caring for diabetes haven’t yet significantly changed personal behavior relative to the key risks for Type 2 diabetes amenable to change: food intake and exercise.
The rising costs of caring for diabetes haven’t yet significantly changed personal behavior relative to the key risks for Type 2 diabetes amenable to change: food intake and exercise.