In December, CMS listed its quality measures that it is considering for incorporation into some of their value-based payment programs and quality reporting programs. However, which Medicare quality reporting and payment initiatives use quality measures? A full list is below.
- Ambulatory Surgical Center Quality Reporting Program (ASCQR)
- End-Stage Renal Disease Quality Incentive Program (ESRD QIP)
- Home Health Quality Reporting Program (HH QRP)
- Hospice Quality Reporting Program (HQRP)
- Hospital-Acquired Condition Reduction Program (HACRP)
- Hospital Inpatient Quality Reporting Program (HIQR)
- Hospital Outpatient Quality Reporting Program (HOQR)
- Hospital Readmissions Reduction Program (HRRP)
- Hospital Value-Based Purchasing Program (HVBP)
- Inpatient Psychiatric Facility Quality Reporting Program (IPFQR)
- Inpatient Rehabilitation Facility Quality Reporting Program (IRF QRP)
- Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
- Medicare and Medicaid EHR Incentive Program for Eligible Hospitals (EHs) and Critical Access Hospitals (CAHs)
- Medicare Shared Savings Program (MSSP)
- Merit-based Incentive Payment System (MIPS)
- Prospective Payment System (PPS)-Exempt Cancer Hospital Quality Reporting Program (PCHQR)
- Skilled Nursing Facility Quality Reporting Program (SNF QRP)
- Skilled Nursing Facility Value-Based Purchasing Program (SNF VBP)
One can readily see how these quality-based programs, while well-intentioned could be problematic for providers. A hospital that is part of an ACO that provides inpatient, outpatient and psychiatric and rehabilitatoin facilities would be subject to quality reporting for HACRP, HIQR, HOQR, HRRP, HVBP, IPFQR, IRF QRP, and MSSP. That is a lot of quality reporting.
Another question you may have are whether these measures are any good. Most measures are NQF endorsed. Further, a number of other of government agencies have provided input on these measures. A full list of agencies providing input is below.
- Office of the Assistant Secretary for Health (OASH)
- Office of the National Coordinator for Health Information Technology (ONC)
- National Institutes of Health (NIH)
- Agency for Healthcare Research and Quality (AHRQ)
- Health Resources and Services Administration (HRSA)
- Centers for Disease Control and Prevention (CDC)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Office of the Assistant Secretary for Planning and Evaluation (ASPE)
- Indian Health Service (IHS)
In short, getting from volume to value-based payment, ultimately depends on being able to accurately measure quality. Measuring quality is a lot easier to do in theory than in practice.
Which Medicare initiatives use quality measures? posted first on http://dentistfortworth.blogspot.com
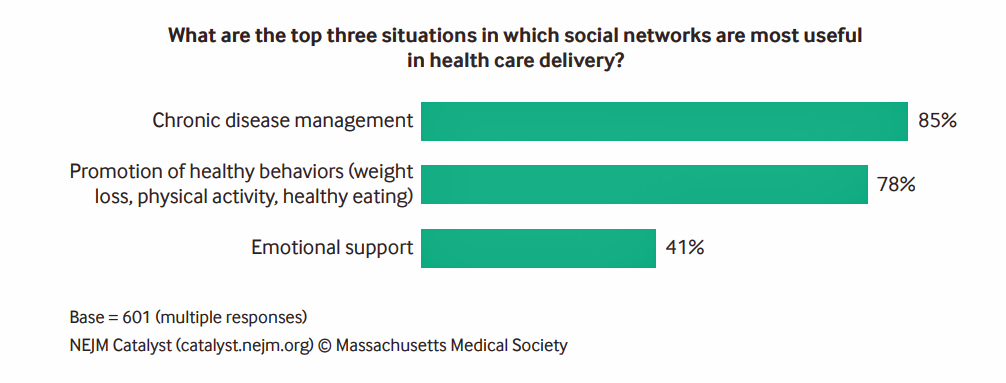
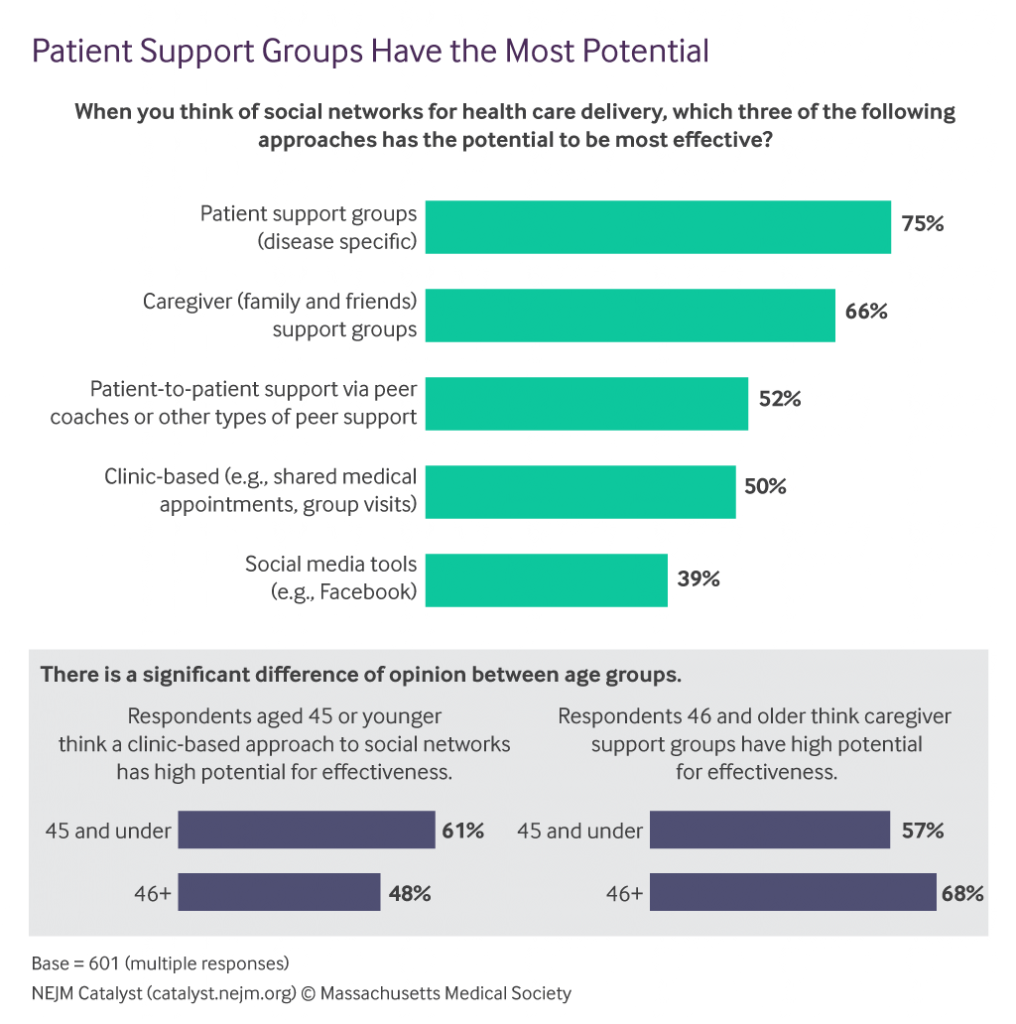 “Awareness is growing that social networks in health care…can help people improve health behaviors. Peer networks can provide information and community to patients who otherwise might struggle alone with a new or existing disease,” Dr. Kevin Volpp of University of Pennsylvania and Dr. Namita Mohta of Brigham and Women’s Hospital co-write in the report.
“Awareness is growing that social networks in health care…can help people improve health behaviors. Peer networks can provide information and community to patients who otherwise might struggle alone with a new or existing disease,” Dr. Kevin Volpp of University of Pennsylvania and Dr. Namita Mohta of Brigham and Women’s Hospital co-write in the report.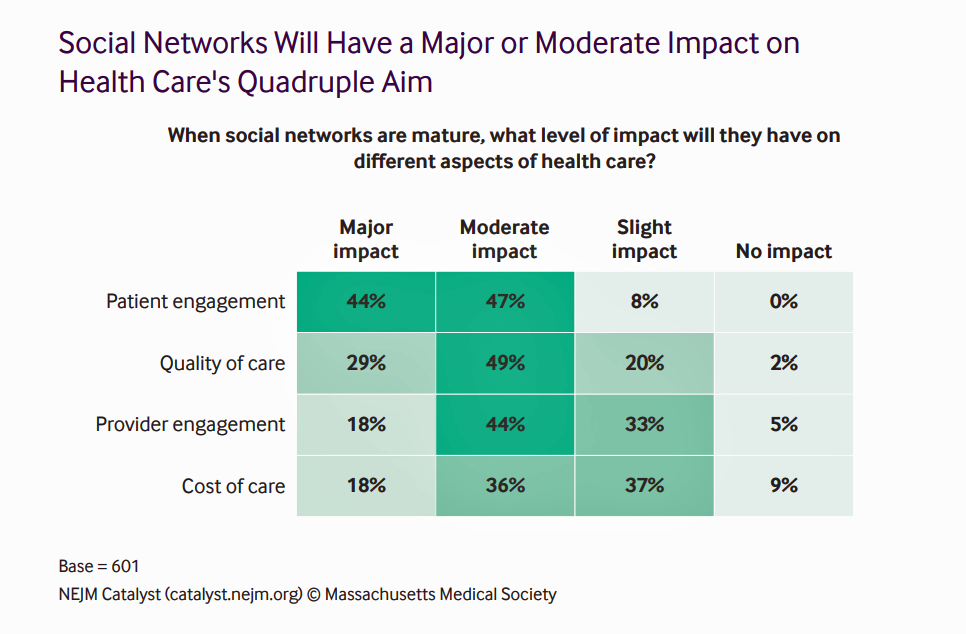 How impactful might social networks be on different aspects of health care? The biggest impacts, Catalyst members say, will be on patient engagement, quality of care, and provider engagement. Over one-half of providers believe social networks, once mature, would also impact the cost of care in a moderate or major way.
How impactful might social networks be on different aspects of health care? The biggest impacts, Catalyst members say, will be on patient engagement, quality of care, and provider engagement. Over one-half of providers believe social networks, once mature, would also impact the cost of care in a moderate or major way.
 Over four in 10 U.S. workers were enrolled in a high-deductible health plan in the first 9 months of 2017,
Over four in 10 U.S. workers were enrolled in a high-deductible health plan in the first 9 months of 2017, 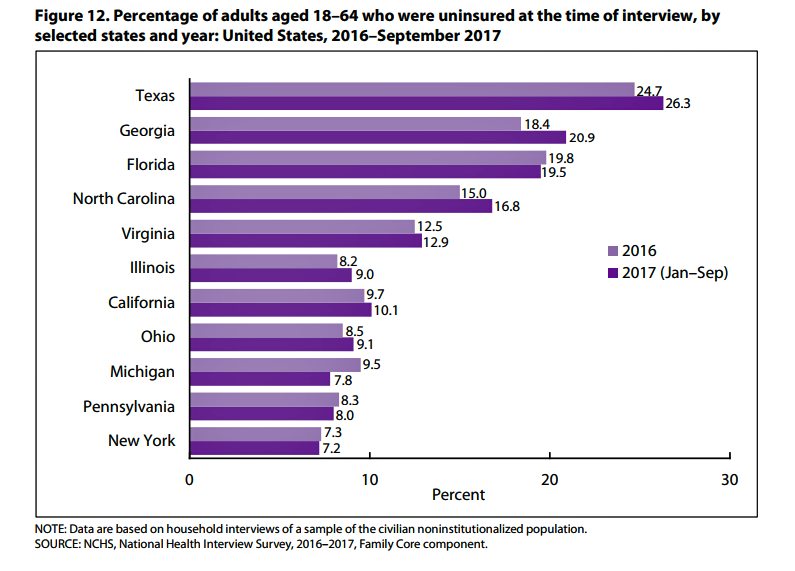
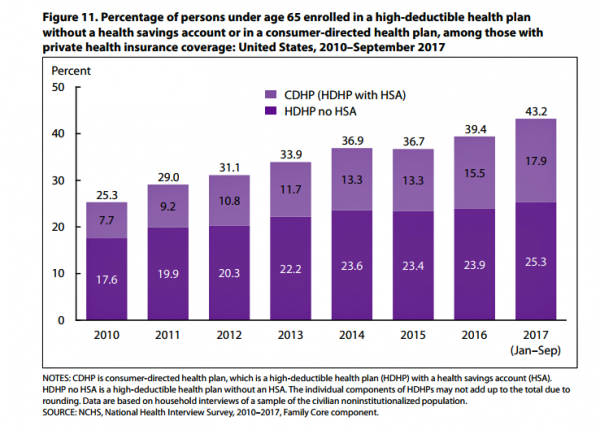 The third chart illustrates the growth in high-deductible health plans (HDHPs) with and without health savings accounts (HSAs). In the first nine months of 2017, 43.2% of working-age people (under 65 years of age) were enrolled in an HDHP: 18% in consumer-directed health plans (which are HDHPs bundled with an HSA) and 25% in an HDHP (which do not have an HSA with the plan).
The third chart illustrates the growth in high-deductible health plans (HDHPs) with and without health savings accounts (HSAs). In the first nine months of 2017, 43.2% of working-age people (under 65 years of age) were enrolled in an HDHP: 18% in consumer-directed health plans (which are HDHPs bundled with an HSA) and 25% in an HDHP (which do not have an HSA with the plan). There are more tools available for patients-consumers who choose to shop for services; just this week in my own town of Philadelphia, Clear Health Costs launched Philly Price Check through two local media outlets,
There are more tools available for patients-consumers who choose to shop for services; just this week in my own town of Philadelphia, Clear Health Costs launched Philly Price Check through two local media outlets,  If played out well, the combination could become an important player in the evolving U.S. health/care ecosystem that brings a self-care front-door closer to consumers, patients and caregivers.
If played out well, the combination could become an important player in the evolving U.S. health/care ecosystem that brings a self-care front-door closer to consumers, patients and caregivers.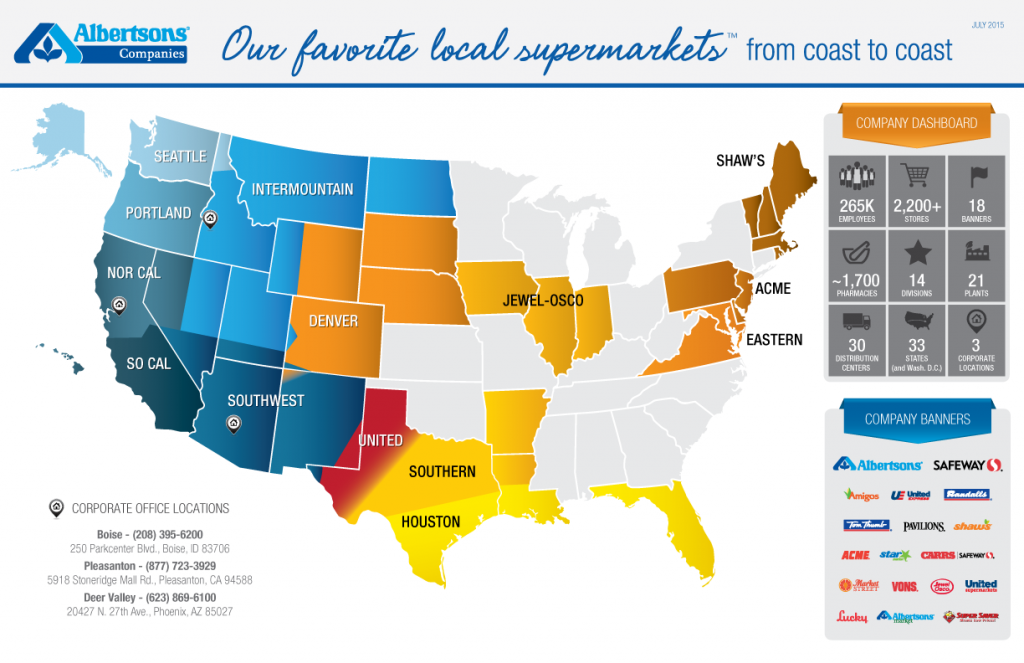 Albertsons’ geographic footprint has been heavily weighted on the western side of America, with some Mid-Atlantic reach through the Acme, Eastern and Shaws storefronts. Adding Rite Aid to this map would expand Albertsons’ physical reach to millions of more food, healthcare and wellness consumers.
Albertsons’ geographic footprint has been heavily weighted on the western side of America, with some Mid-Atlantic reach through the Acme, Eastern and Shaws storefronts. Adding Rite Aid to this map would expand Albertsons’ physical reach to millions of more food, healthcare and wellness consumers.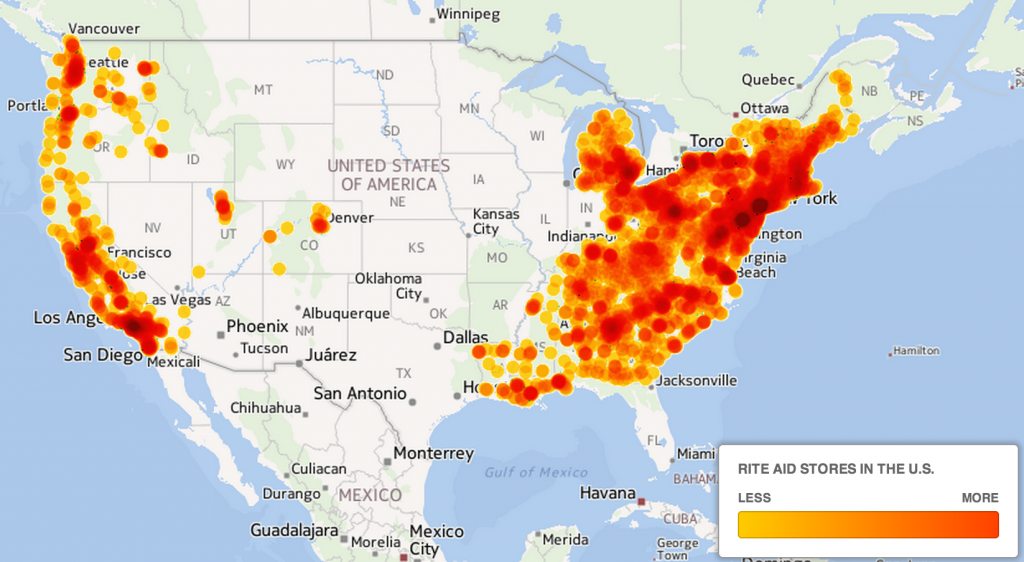 Rite Aid has a concentration of bricks-and-mortar stores east of the Mississippi, as the second map illustrates.
Rite Aid has a concentration of bricks-and-mortar stores east of the Mississippi, as the second map illustrates.
 Change Healthcare published the company’s
Change Healthcare published the company’s  One of my favorite series of papers that inform my advisory work comes from PwC on the New Health Economy, this week publishing its report on
One of my favorite series of papers that inform my advisory work comes from PwC on the New Health Economy, this week publishing its report on 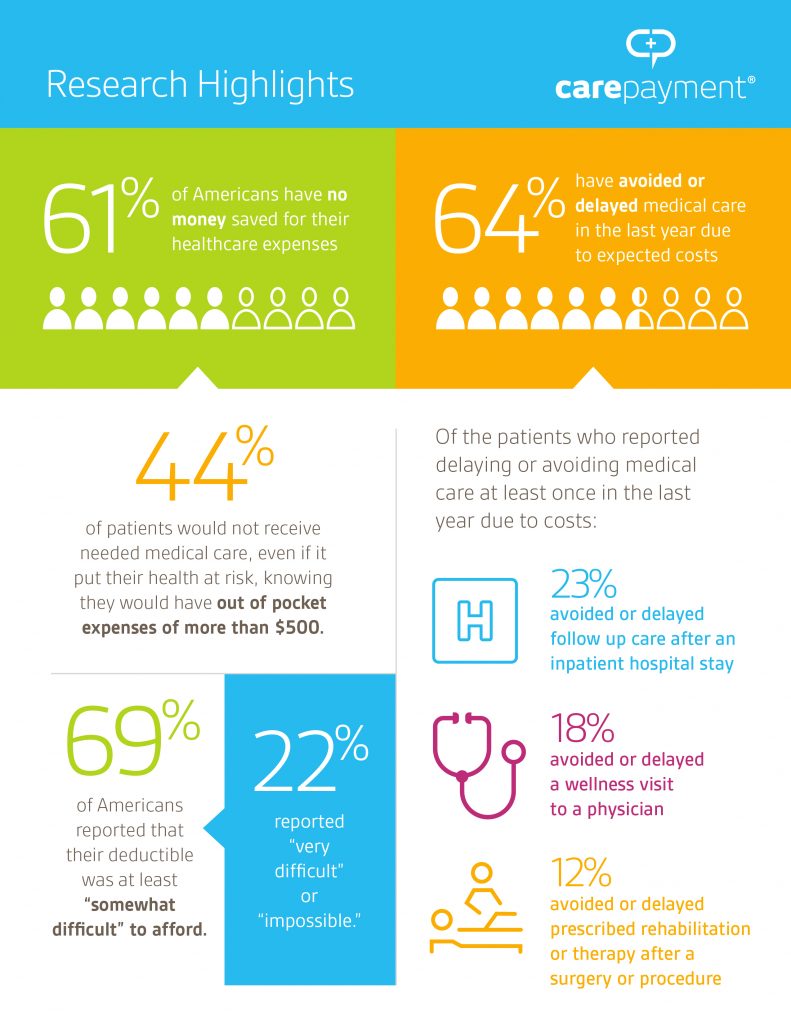 Finally,
Finally, 
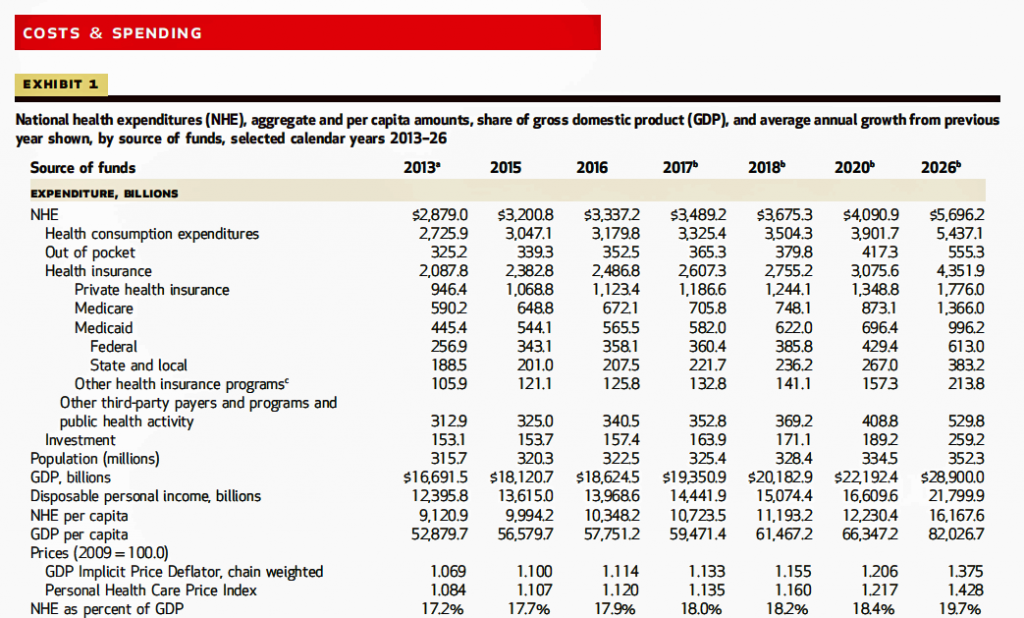 I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled,
I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled, 
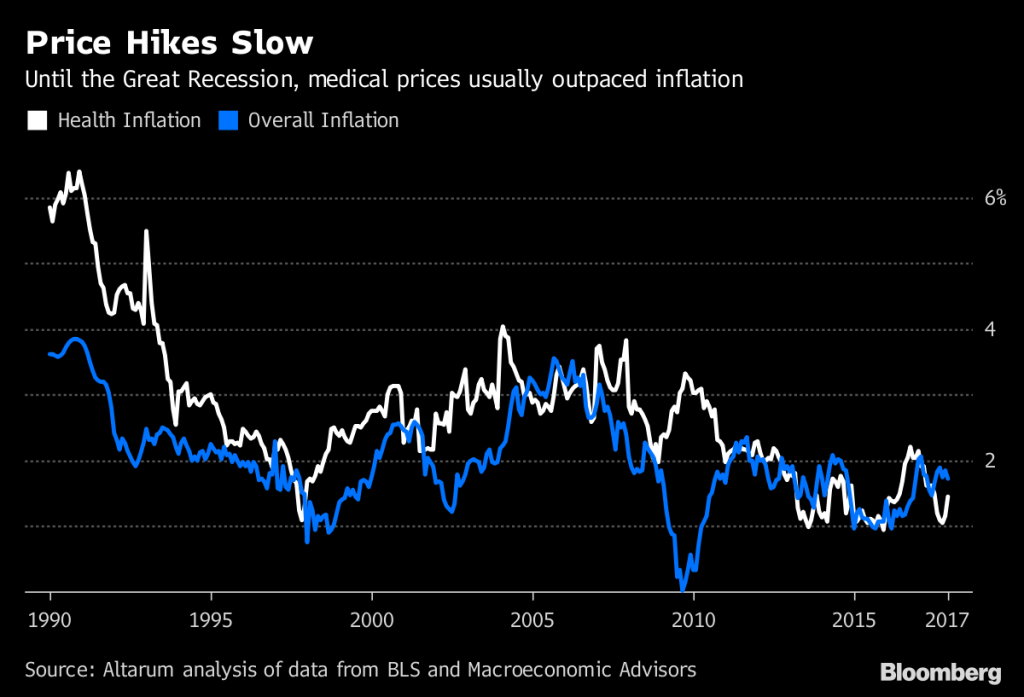 Altarum Institute informed
Altarum Institute informed 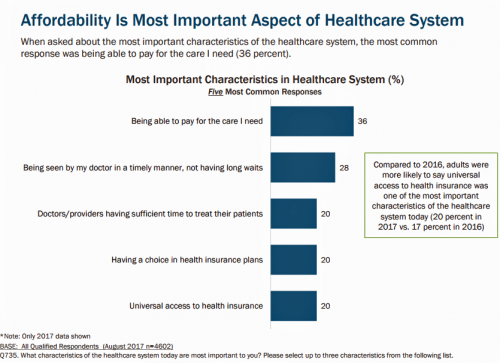 Through the eyes of the American patient, now health consumer, affordability continues to rank ahead of quality or access for health care based on TransAmerica’s research into healthcare consumers in a time of uncertainty. Underpinning affordability concerns is 70% of consumers’ confession that they do not currently save for healthcare expenses.
Through the eyes of the American patient, now health consumer, affordability continues to rank ahead of quality or access for health care based on TransAmerica’s research into healthcare consumers in a time of uncertainty. Underpinning affordability concerns is 70% of consumers’ confession that they do not currently save for healthcare expenses.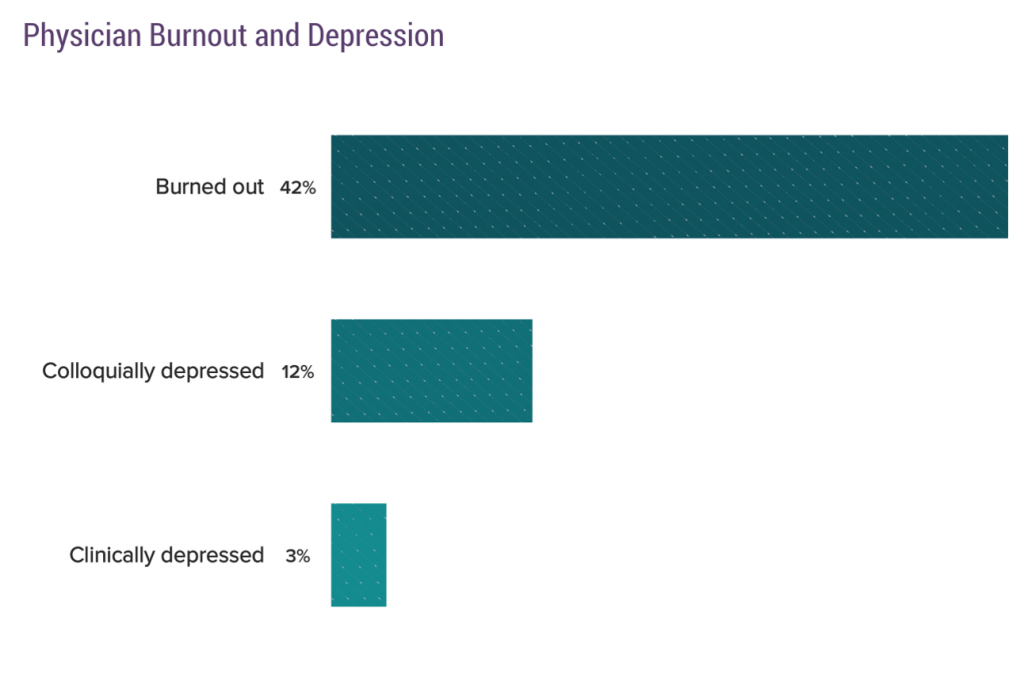 Healthcare providers are the front-line stakeholders who, increasingly, are taking on payment and incentives to help manage individual patient and communities’ health. More hospitals are physicians’ employers, and so bear the responsibility of supporting doctors and nurses in working to their highest and best use – especially empowering professionals in their patient care missions. The
Healthcare providers are the front-line stakeholders who, increasingly, are taking on payment and incentives to help manage individual patient and communities’ health. More hospitals are physicians’ employers, and so bear the responsibility of supporting doctors and nurses in working to their highest and best use – especially empowering professionals in their patient care missions. The  Still, clinicians need to
Still, clinicians need to 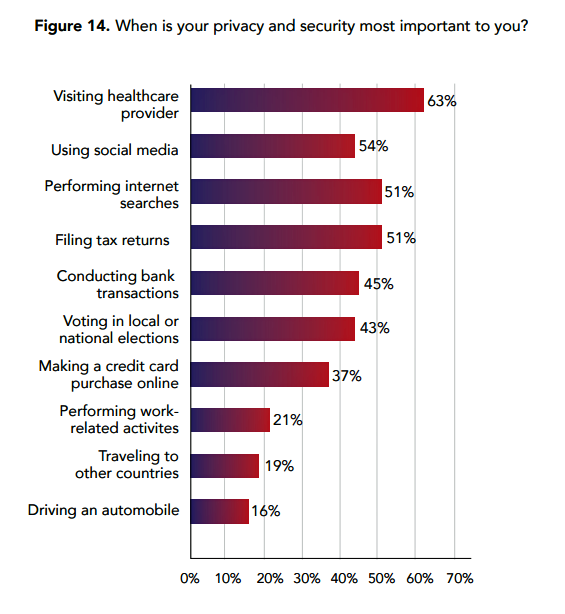 Most consumers say
Most consumers say 
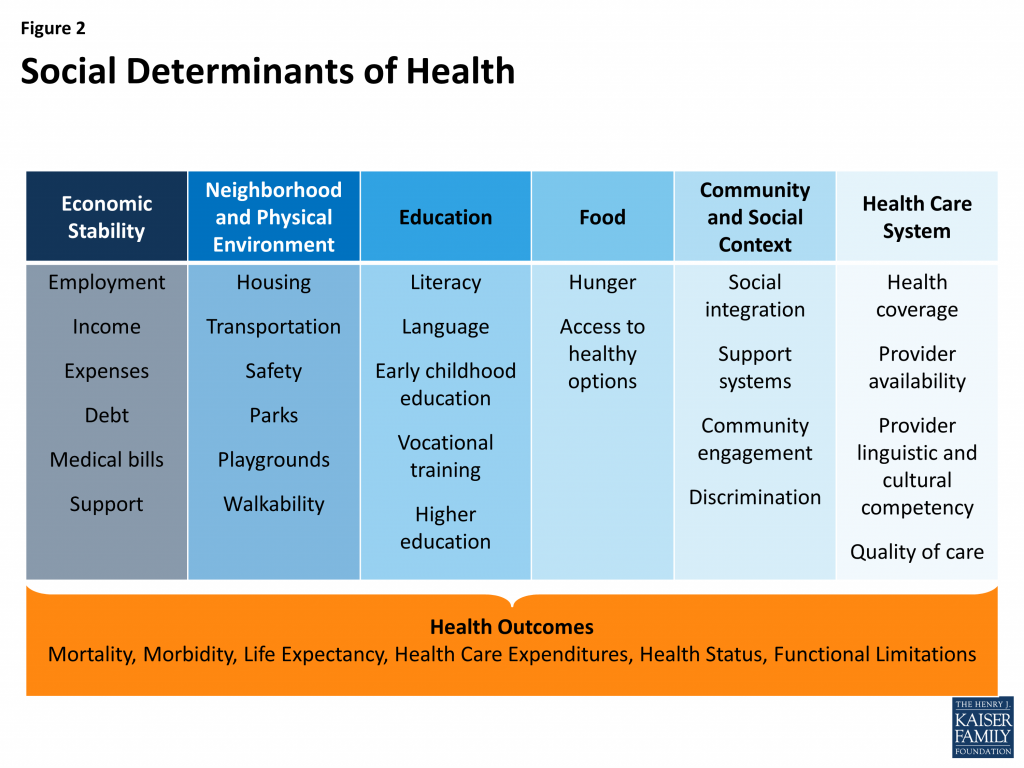 To remind you about the social determinants, here’s a graphic from Kaiser Family Foundation that summarizes the key pillars of SDOH.
To remind you about the social determinants, here’s a graphic from Kaiser Family Foundation that summarizes the key pillars of SDOH. Assumption 2: Providing transportation to/from health care services will bolster patients’ appointment-making. About 3.6 million U.S. adults miss medical appointments each year due to transportation challenges, many of whom earn lower incomes. A
Assumption 2: Providing transportation to/from health care services will bolster patients’ appointment-making. About 3.6 million U.S. adults miss medical appointments each year due to transportation challenges, many of whom earn lower incomes. A 
 Those “other barriers” can include financial — a top consumer health issue with which regular Health Populi readers will be well aware — along with cultural preferences, job and work commitments (limiting time to seek care inside of “regular” operating hours), and institutional barriers such as racial and ethnic factors that prevent some people trusting healthcare institutions.
Those “other barriers” can include financial — a top consumer health issue with which regular Health Populi readers will be well aware — along with cultural preferences, job and work commitments (limiting time to seek care inside of “regular” operating hours), and institutional barriers such as racial and ethnic factors that prevent some people trusting healthcare institutions.