Tuesday, 31 October 2017
Monday, 30 October 2017
Improving catchment area definitions when measuring quality of care
Oftentimes, we want to measure the quality of care of a give hospital or health care system. The easiest way of doing this is to measure the quality of care received by patients who go to that hospital. These patients, however, may attend multiple hospitals during they year. Further, if quality of care includes avoiding hospitalizations, we need to identify not only patients who had a hospital admission but patients who were at risk of going to that hospital if a preventable admission occurred.
One way to model quality of care is to use catchment areas. Catchment areas are typically aggregations of geographic units. For instance, hospital service areas (HSAs) are aggregations of ZIP codes. However, previous research has shown that HSA-based catchment areas only capturing 50% to 80% of hospital admissions for their given population. One could use larger geographic regions—such as hospital referral regions (HRRs)—but then one is susceptible to assigning patients to hospitals over which they are unlikely to have responsibility for their care.
My previous research on the hospital wage index (see here and here) proposed assigning a weighting of the geographic units While that approach aimed to measure geographic variation in wages where data was available by geography rather than by person, an interesting paper by Falster, Jorn and Leyland (2017) proposes a different approach using individual patient data and a methodology known as multiple-membership multi-level model multi-level.
To explain this model, consider first a standard approach whereby where I people are clustered within J hospitals or HSAs.
Yij is the outcome, xpi are the regression parameters for P person-level variables, and xqj are the regression parameters for Q hospital-level variables. This multilevel model captures the effects of clustering by allowing both regression parameters and error terms to exist at different hierarchical levels.
A multiple-membership multilevel model extends this approach by allowing a weighted structure for each of the hospital-level components as follows:
Here, the superscripts represent the different model hierarchy levels. Faster and co-authors apply this model to date on preventable hospitalizations in NSW Australia using weighted hospital service area networks (weighted-HSANs). The authors contend that:
Between-hospital variation in rates of preventable hospitalization was more than two times greater when modeled using weighted-HSANs rather than HSAs. Use of weighted-HSANs permitted identification of small hospitals with particularly high rates of admission and influenced performance ranking of hospitals, particularly those with a broadly distributed patient base.
While this approach is a significant improvement for an academic setting, it is problematic to operationalize in terms of quality improvement. In order to improve quality, hospitals need clear rules regarding the patients to which it is attributed. While the authors compellingly argue that multiple-membership multilevel models do a better job mof measuring quality retrospectively than would be the case using HSAs alone, operationalizing the use of weighted HSANs in practice would be more difficult due to the model complexity. Nevertheless, this approach clearly highlights the challenges of using HAS-based catchment areas to measure quality of care.
Source:
- Falster, Michael O., Louisa R. Jorm, and Alastair H. Leyland. “Using Weighted Hospital Service Area Networks to Explore Variation in Preventable Hospitalization.” Health Services Research (2017).
Improving catchment area definitions when measuring quality of care posted first on http://ift.tt/2sNcj5z
Sunday, 29 October 2017
How to pay for cures
Do you want to cure cancer? Diabetes? HIV? Imagine if there was a single pill for each of these diseases that one could take to cure the diseases. That would be a clear clinical advance, it would save lives, and also save money form reducing the cost of treating these disease.
Can we expect to see these cures? This is partly a question of science and partly a question of finance. On the science side, curing complex diseases is difficult and this fact should not be underestimated. On the finance side, however, innovators have less an incentive to invent cures than to invent treatments. For instance, let us say that someone had a drug that would treat diabetes, but patients had to pay $1000 per month over 50 years (60 months) in order to keep the disease in reemission. This means that patients and health plans will spend $600,000 ($1000 x 50 years x 12 months) over this time period. If someone could invent a drug that had the same efficacy in terms of long-term, 50-year disease remission, the treatment would be worth at least $600,000. However, health plans may not be able to afford spending $600,000 per patient in the short-run. Even if they could afford this price, many health plan enrollees leave the system after only a few years and thus health plans that pay for the $600,000 will not accrue the full benefit.
One clear solution to the first issue is to just finance the purchase of the cure with debt. Many individuals want to own a house, but most people cannot afford to make a lump sum payment for the house. The solution is that people take out a mortgage and spread the payments over time. Tomas Philipson and Andrew von Eschenbach have proposed debt financings of high-value cures. This approach, however, does not solve the free rider problem that occurs if there is frequent health plan turnover.
Another innovation is the concept of a HealthCoin developed by Basu (2015). In this approach, the health advantages of a cure turn into an asset. For instance, by giving someone Sovaldi to cure Hepatitis C, a health plan could earn a “HealthCoin.” If a person who received Sovaldi later leaves the plan, he new plan where the person was enrolled would need to pay the original plan the value of the HealthCoin. A more general description is below from Yeung et al. (2017).
HealthCoin is a potential tradable currency that would be backed by Medicare, wherein Medicare guarantees payment to the private payer for each treated person entering the Medicare program.20 This option incentivizes private payers to invest in upfront coverage for cures, since cured individuals would likely have lower morbidity, and the private payer can sell the remaining value of the HealthCoins when the member switches plans
Although the concept of a HealthCoin may seem esoteric, managed care pharmacists seem to appreciate the value of this idea, once it is clearly explained to them.
Regardless if you think HealthCoins are the right answer, we need to have the right incentives in place to make sure innovators have the incentive to develop cures for highly prevalent, high-burden diseases.
How to pay for cures posted first on http://ift.tt/2sNcj5z
Will CVS buy Aetna for $66 billion?
CVS is in talks to buy Aetna for $66 billion. This would be a merger between one of the largest pharmacy benefits managers (PBM) in the country and the third largest insurer.
A successful deal could push millions of Aetna’s members toward CVS’s retail pharmacies, walk-in Minute Clinics, and services such as home visits for infusion drugs at a time when retail pharmacy companies are facing stiff competition.
It would also give Aetna the ability to move deeper into the lives of the 44.7 million people it serves and manage their health more efficiently. For example, the insurer might be able to get better insight into whether patients are taking their drugs by gaining access to data from CVS clinics and retail counters.
However, there may be another reason for the deal. Amazon may be entering the medical device and even eventually the PBM business.
Amazon has received approval for wholesale pharmacy licenses in at least 12 states, including Nevada, Arizona, North Dakota, Louisiana, Alabama, New Jersey, Michigan, Connecticut, Idaho, New Hampshire, Oregon and Tennessee.
However, the CVS-Aetna deal may never happen. According to Bruce Japsen of Forbes:
Anthem just last week said it was forming its own pharmacy benefit management company, IngenioRx, with CVS, which operates a PBM. That was seen as a way to compete with the nation’s largest health insurer, UnitedHealth Group, which owns the PBM OptumRx.
But for CVS to operate a PBM with Anthem, the No. 2 health insurer, while owning Aetna, the No. 3 insurer, would be highly unusual coming off a period of intense antitrust scrutiny of the health insurance industry. Aetna and Humana, the nation’s fourth-largest insurer, pulled the plug on their merger last year after intense antitrust scrutiny over the potential creation of a monopoly purchaser of health services.
The health care market is rapidly evolving. In the words of Heraclitus, “you cannot step twice into the same stream” or put more simply, “The only thing that is constant is change“.
Will CVS buy Aetna for $66 billion? posted first on http://ift.tt/2sNcj5z
HWR is up
Health Wonk Review: Disaster edition is freshly posted by David Williams at the Health Business Blog. Check it out!
HWR is up posted first on http://ift.tt/2sNcj5z
How much is your life worth?
According to the Environmental Protection Agency, the answer is $10 million. Other agencies place use a somewhat lower number. The Food and Drug administration pegs the value at $9.5 million and the Department of Agriculture places the value at $8.9 million.
Technically, what these agencies are calculating are the value of a statistical life (VSL). Although measuring the value of a life is an interesting academic exercise, it has real world implications. Notably, VSL is used in federal agencies cost benefit analyses.
For instance, consider a new regulation to reduce pollution that saves 10 lives but costs $50 million. Should society undertake this intervention? If VSL is $10 million, then the answer is ‘yes.’ Each of the 10 lives is worth $10 million so the regulation leads to $100 million in benefits but only costs $50 million.
On the other hand, consider a more drastic intervention for reducing population: making privately owned cars illegal. In this case, let us say the intervention saved 10 lives still but the cost now is $1 billion is lost economic activity. In this second example, the costs outweigh the benefits and so based pursed on aggregated costs and benefits, we would not implement this intervention.
For the politically minded, those who prefer more regulation would prefer a higher VSL and those who prefer less regulaion would opt for a lower VSL.
How much is your life worth? posted first on http://ift.tt/2sNcj5z
Improving catchment area definitions when measuring quality of care
Oftentimes, we want to measure the quality of care of a give hospital or health care system. The easiest way of doing this is to measure the quality of care received by patients who go to that hospital. These patients, however, may attend multiple hospitals during they year. Further, if quality of care includes avoiding hospitalizations, we need to identify not only patients who had a hospital admission but patients who were at risk of going to that hospital if a preventable admission occurred.
One way to model quality of care is to use catchment areas. Catchment areas are typically aggregations of geographic units. For instance, hospital service areas (HSAs) are aggregations of ZIP codes. However, previous research has shown that HSA-based catchment areas only capturing 50% to 80% of hospital admissions for their given population. One could use larger geographic regions—such as hospital referral regions (HRRs)—but then one is susceptible to assigning patients to hospitals over which they are unlikely to have responsibility for their care.
My previous research on the hospital wage index (see here and here) proposed assigning a weighting of the geographic units While that approach aimed to measure geographic variation in wages where data was available by geography rather than by person, an interesting paper by Falster, Jorn and Leyland (2017) proposes a different approach using individual patient data and a methodology known as multiple-membership multi-level model multi-level.
To explain this model, consider first a standard approach whereby where I people are clustered within J hospitals or HSAs.
Yij is the outcome, xpi are the regression parameters for P person-level variables, and xqj are the regression parameters for Q hospital-level variables. This multilevel model captures the effects of clustering by allowing both regression parameters and error terms to exist at different hierarchical levels.
A multiple-membership multilevel model extends this approach by allowing a weighted structure for each of the hospital-level components as follows:
Here, the superscripts represent the different model hierarchy levels. Faster and co-authors apply this model to date on preventable hospitalizations in NSW Australia using weighted hospital service area networks (weighted-HSANs). The authors contend that:
Between-hospital variation in rates of preventable hospitalization was more than two times greater when modeled using weighted-HSANs rather than HSAs. Use of weighted-HSANs permitted identification of small hospitals with particularly high rates of admission and influenced performance ranking of hospitals, particularly those with a broadly distributed patient base.
While this approach is a significant improvement for an academic setting, it is problematic to operationalize in terms of quality improvement. In order to improve quality, hospitals need clear rules regarding the patients to which it is attributed. While the authors compellingly argue that multiple-membership multilevel models do a better job mof measuring quality retrospectively than would be the case using HSAs alone, operationalizing the use of weighted HSANs in practice would be more difficult due to the model complexity. Nevertheless, this approach clearly highlights the challenges of using HAS-based catchment areas to measure quality of care.
Source:
- Falster, Michael O., Louisa R. Jorm, and Alastair H. Leyland. “Using Weighted Hospital Service Area Networks to Explore Variation in Preventable Hospitalization.” Health Services Research (2017).
Improving catchment area definitions when measuring quality of care posted first on http://ift.tt/2sNcj5z
Health plans getting into the PBM game
Bloomberg reports that Anthem is creating is own pharmacy benefits manager (PBM). Why? It says it wasn’t getting a good deal from PBMs.
Health insurer Anthem Inc. plans to set up its own pharmacy benefits management unit, signaling a final break with Express Scripts Holding Co. after accusing it of overcharging by billions of dollars.
The move means Express Scripts will not only lose its biggest client but also face a new rival. Anthem’s new unit, called IngenioRx, will grow its own business with a “full suite” of services, the insurer said in a statement on Wednesday.
How much was the overcharging? Anthem says the amount was $3 billion.
With drug prices on the rise, both pharma and PBM’s blame each other for high prices. PBMs say that drug list prices are too high. Pharmacetuical firms say they need to raise prices in order to offset large discounts and rebates that PBMs are demanding.
Anthem may not be the only firm entering the PBM market. Amazon is also considering entering the PBM market. UnitedHealth–Anthem’s top competitor–already has an in-house PBM known as OptumRx.
The one thing that is certain in the PBM world is that things are changing.
Health plans getting into the PBM game posted first on http://ift.tt/2sNcj5z
Friday, 27 October 2017
Will CVS buy Aetna for $66 billion?
CVS is in talks to buy Aetna for $66 billion. This would be a merger between one of the largest pharmacy benefits managers (PBM) in the country and the third largest insurer.
A successful deal could push millions of Aetna’s members toward CVS’s retail pharmacies, walk-in Minute Clinics, and services such as home visits for infusion drugs at a time when retail pharmacy companies are facing stiff competition.
It would also give Aetna the ability to move deeper into the lives of the 44.7 million people it serves and manage their health more efficiently. For example, the insurer might be able to get better insight into whether patients are taking their drugs by gaining access to data from CVS clinics and retail counters.
However, there may be another reason for the deal. Amazon may be entering the medical device and even eventually the PBM business.
Amazon has received approval for wholesale pharmacy licenses in at least 12 states, including Nevada, Arizona, North Dakota, Louisiana, Alabama, New Jersey, Michigan, Connecticut, Idaho, New Hampshire, Oregon and Tennessee.
However, the CVS-Aetna deal may never happen. According to Bruce Japsen of Forbes:
Anthem just last week said it was forming its own pharmacy benefit management company, IngenioRx, with CVS, which operates a PBM. That was seen as a way to compete with the nation’s largest health insurer, UnitedHealth Group, which owns the PBM OptumRx.
But for CVS to operate a PBM with Anthem, the No. 2 health insurer, while owning Aetna, the No. 3 insurer, would be highly unusual coming off a period of intense antitrust scrutiny of the health insurance industry. Aetna and Humana, the nation’s fourth-largest insurer, pulled the plug on their merger last year after intense antitrust scrutiny over the potential creation of a monopoly purchaser of health services.
The health care market is rapidly evolving. In the words of Heraclitus, “you cannot step twice into the same stream” or put more simply, “The only thing that is constant is change“.
Will CVS buy Aetna for $66 billion? posted first on http://ift.tt/2sNcj5z
Health plans getting into the PBM game
Bloomberg reports that Anthem is creating is own pharmacy benefits manager (PBM). Why? It says it wasn’t getting a good deal from PBMs.
Health insurer Anthem Inc. plans to set up its own pharmacy benefits management unit, signaling a final break with Express Scripts Holding Co. after accusing it of overcharging by billions of dollars.
The move means Express Scripts will not only lose its biggest client but also face a new rival. Anthem’s new unit, called IngenioRx, will grow its own business with a “full suite” of services, the insurer said in a statement on Wednesday.
How much was the overcharging? Anthem says the amount was $3 billion.
With drug prices on the rise, both pharma and PBM’s blame each other for high prices. PBMs say that drug list prices are too high. Pharmacetuical firms say they need to raise prices in order to offset large discounts and rebates that PBMs are demanding.
Anthem may not be the only firm entering the PBM market. Amazon is also considering entering the PBM market. UnitedHealth–Anthem’s top competitor–already has an in-house PBM known as OptumRx.
The one thing that is certain in the PBM world is that things are changing.
Health plans getting into the PBM game posted first on http://ift.tt/2sNcj5z
Quotation of the Day
To achieve greatness, two things are needed: a plan and not quite enough time
- Leonard Bernstein
Quotation of the Day posted first on http://ift.tt/2sNcj5z
Improving catchment area definitions when measuring quality of care
Oftentimes, we want to measure the quality of care of a give hospital or health care system. The easiest way of doing this is to measure the quality of care received by patients who go to that hospital. These patients, however, may attend multiple hospitals during they year. Further, if quality of care includes avoiding hospitalizations, we need to identify not only patients who had a hospital admission but patients who were at risk of going to that hospital if a preventable admission occurred.
One way to model quality of care is to use catchment areas. Catchment areas are typically aggregations of geographic units. For instance, hospital service areas (HSAs) are aggregations of ZIP codes. However, previous research has shown that HSA-based catchment areas only capturing 50% to 80% of hospital admissions for their given population. One could use larger geographic regions—such as hospital referral regions (HRRs)—but then one is susceptible to assigning patients to hospitals over which they are unlikely to have responsibility for their care.
My previous research on the hospital wage index (see here and here) proposed assigning a weighting of the geographic units While that approach aimed to measure geographic variation in wages where data was available by geography rather than by person, an interesting paper by Falster, Jorn and Leyland (2017) proposes a different approach using individual patient data and a methodology known as multiple-membership multi-level model multi-level.
To explain this model, consider first a standard approach whereby where I people are clustered within J hospitals or HSAs.
Yij is the outcome, xpi are the regression parameters for P person-level variables, and xqj are the regression parameters for Q hospital-level variables. This multilevel model captures the effects of clustering by allowing both regression parameters and error terms to exist at different hierarchical levels.
A multiple-membership multilevel model extends this approach by allowing a weighted structure for each of the hospital-level components as follows:
Here, the superscripts represent the different model hierarchy levels. Faster and co-authors apply this model to date on preventable hospitalizations in NSW Australia using weighted hospital service area networks (weighted-HSANs). The authors contend that:
Between-hospital variation in rates of preventable hospitalization was more than two times greater when modeled using weighted-HSANs rather than HSAs. Use of weighted-HSANs permitted identification of small hospitals with particularly high rates of admission and influenced performance ranking of hospitals, particularly those with a broadly distributed patient base.
While this approach is a significant improvement for an academic setting, it is problematic to operationalize in terms of quality improvement. In order to improve quality, hospitals need clear rules regarding the patients to which it is attributed. While the authors compellingly argue that multiple-membership multilevel models do a better job mof measuring quality retrospectively than would be the case using HSAs alone, operationalizing the use of weighted HSANs in practice would be more difficult due to the model complexity. Nevertheless, this approach clearly highlights the challenges of using HAS-based catchment areas to measure quality of care.
Source:
- Falster, Michael O., Louisa R. Jorm, and Alastair H. Leyland. “Using Weighted Hospital Service Area Networks to Explore Variation in Preventable Hospitalization.” Health Services Research (2017).
Improving catchment area definitions when measuring quality of care posted first on http://ift.tt/2sNcj5z
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update
Last week, President Trump once again used the “M” word (“murder”) in a sentence accusing the pharmaceutical industry of too-high priced products for U.S. health citizens. The sentence included the phrase, “Drug companies are getting away with murder.” That week, USA Today published an article on a new FDA-approved specialty drug therapy that could add up to over a $1 mm price tag.
There is much to report in the world of pharmaceutical innovation, pricing, and patient Rx coverage this month. The CVS Health – Epic announcement ranks high in Health Populi’s vision for the evolving health/care ecosystem, bringing together two key industry leaders in their segments: retail pharmacy and prescription benefits management, and healthcare information technology. Each of these companies is the largest in their sector, and therefore brings scale and reach to this collaboration that aims to lower the cost of prescription drugs to plan members while bolstering medication adherence — two Holy Grails of healthcare in the current constrained health economy. The program has a strong population health focus, as well as a broad view on retail data to be included in the electronic health record: over-the-counter meds purchased in the “front of the store” will also be included in the patient’s EHR, allowing clinicians to have a more complete view of a person’s real-life medicines and supplements list.
On the drug-pricing front, PwC published its paper on Launching into Value, discussing pharma’s “quest” to align drug prices with outcomes. Broadly-defined, value has already come to health care and the concept will expand for both public payors (Medicare in 2018, and state Medicaid programs in various ways), and among commercial payors. Note that the Health Care Transformation Task Force, composed of major payors, purchasers, and patient advocacy groups, has committed to move 75% of the group’s collection business into value-based payment programs by 2020. PwC’s survey of pharmaceutical industry executives found that while the stakeholders are aware of value-based trends, only one-third of pharma execs believe the rewards of the programs align with the risks companies take in entering these contracts.
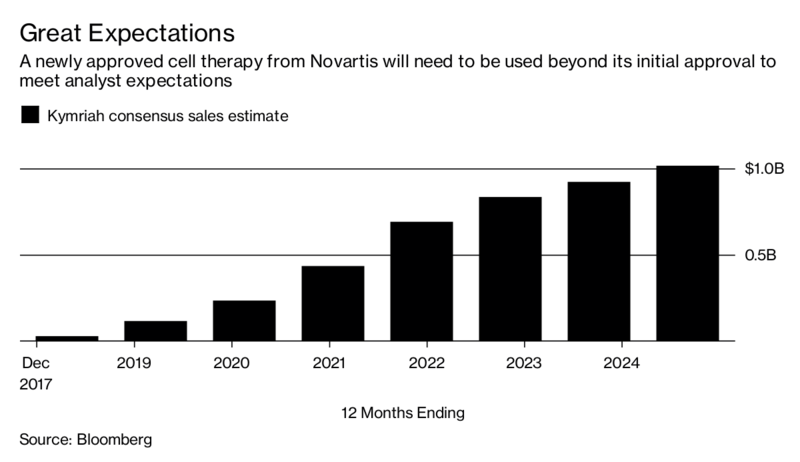 What is the value of a $1 mm therapy? That would be in the eye of the beholder: if you are a parent of a young child whose whole life potential lies ahead, $1 mm might look like a good deal. If you’re 75 in stage four of a painful cancel journey, then you might be at peace that life has been good, and enough. The CAR-T treatment branded as Kymriah was approved in August 2017 with a retail price of $475,000. An article in USA Today published last week estimated that the total cost of care under that therapy could reach $1.5 mm, based on the calculations of a leukemia specialist teaching at the University of Texas MD Anderson Cancer Center.
What is the value of a $1 mm therapy? That would be in the eye of the beholder: if you are a parent of a young child whose whole life potential lies ahead, $1 mm might look like a good deal. If you’re 75 in stage four of a painful cancel journey, then you might be at peace that life has been good, and enough. The CAR-T treatment branded as Kymriah was approved in August 2017 with a retail price of $475,000. An article in USA Today published last week estimated that the total cost of care under that therapy could reach $1.5 mm, based on the calculations of a leukemia specialist teaching at the University of Texas MD Anderson Cancer Center.
Now, to the question of affordability in the eyes of the patient. The Commonwealth Fund’s October 2017 issue brief asks the question, “How Well Does Insurance Coverage Protect Consumers From Health Care Costs?” analyzing the Fund’s biennial health insurance survey. I pulled the multi-colored bar chart which illustrates the reality that over two in five underinsured U.S. adults had problems getting healthcare due to cost. 28% of the underinsured did not fill a prescription due to cost.
The Foundation’s report discusses the Affordable Care Act’s positive outcome for gains in U.S. health citizens’ health care coverage and improvements on key indicators of access and reductions in medical bill problems. A study in this month’s Health Affairs has found that in California, peoples’ use of payday loans fell in concert with the expansion of Medicaid via the ACA, resulting in greater financial wellness for health citizens (in the short-term).
Health Populi’s Hot Points: The issue of “under-insurance” is timely given that the President, who has publicly spoken talked at least twice about the too-high cost of prescription drugs, has promoted the use of so-called skinny health plans that can fly under state regulatory radar. Thus the promise of innovative treatments such as CAR-T therapy for children diagnosed with acute lymphoblastic leukemia may just be a promise if pricing, and peoples’ ability to pay for new-and-improved medicines, do not align.
The post President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update appeared first on HealthPopuli.com.
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update posted first on http://ift.tt/2sNcj5z
Health plans getting into the PBM game
Bloomberg reports that Anthem is creating is own pharmacy benefits manager (PBM). Why? It says it wasn’t getting a good deal from PBMs.
Health insurer Anthem Inc. plans to set up its own pharmacy benefits management unit, signaling a final break with Express Scripts Holding Co. after accusing it of overcharging by billions of dollars.
The move means Express Scripts will not only lose its biggest client but also face a new rival. Anthem’s new unit, called IngenioRx, will grow its own business with a “full suite” of services, the insurer said in a statement on Wednesday.
How much was the overcharging? Anthem says the amount was $3 billion.
With drug prices on the rise, both pharma and PBM’s blame each other for high prices. PBMs say that drug list prices are too high. Pharmacetuical firms say they need to raise prices in order to offset large discounts and rebates that PBMs are demanding.
Anthem may not be the only firm entering the PBM market. Amazon is also considering entering the PBM market. UnitedHealth–Anthem’s top competitor–already has an in-house PBM known as OptumRx.
The one thing that is certain in the PBM world is that things are changing.
Health plans getting into the PBM game posted first on http://ift.tt/2sNcj5z
Quotation of the Day
To achieve greatness, two things are needed: a plan and not quite enough time
- Leonard Bernstein
Quotation of the Day posted first on http://ift.tt/2sNcj5z
Thursday, 26 October 2017
Improving catchment area definitions when measuring quality of care
Oftentimes, we want to measure the quality of care of a give hospital or health care system. The easiest way of doing this is to measure the quality of care received by patients who go to that hospital. These patients, however, may attend multiple hospitals during they year. Further, if quality of care includes avoiding hospitalizations, we need to identify not only patients who had a hospital admission but patients who were at risk of going to that hospital if a preventable admission occurred.
One way to model quality of care is to use catchment areas. Catchment areas are typically aggregations of geographic units. For instance, hospital service areas (HSAs) are aggregations of ZIP codes. However, previous research has shown that HSA-based catchment areas only capturing 50% to 80% of hospital admissions for their given population. One could use larger geographic regions—such as hospital referral regions (HRRs)—but then one is susceptible to assigning patients to hospitals over which they are unlikely to have responsibility for their care.
My previous research on the hospital wage index (see here and here) proposed assigning a weighting of the geographic units While that approach aimed to measure geographic variation in wages where data was available by geography rather than by person, an interesting paper by Falster, Jorn and Leyland (2017) proposes a different approach using individual patient data and a methodology known as multiple-membership multi-level model multi-level.
To explain this model, consider first a standard approach whereby where I people are clustered within J hospitals or HSAs.
Yij is the outcome, xpi are the regression parameters for P person-level variables, and xqj are the regression parameters for Q hospital-level variables. This multilevel model captures the effects of clustering by allowing both regression parameters and error terms to exist at different hierarchical levels.
A multiple-membership multilevel model extends this approach by allowing a weighted structure for each of the hospital-level components as follows:
Here, the superscripts represent the different model hierarchy levels. Faster and co-authors apply this model to date on preventable hospitalizations in NSW Australia using weighted hospital service area networks (weighted-HSANs). The authors contend that:
Between-hospital variation in rates of preventable hospitalization was more than two times greater when modeled using weighted-HSANs rather than HSAs. Use of weighted-HSANs permitted identification of small hospitals with particularly high rates of admission and influenced performance ranking of hospitals, particularly those with a broadly distributed patient base.
While this approach is a significant improvement for an academic setting, it is problematic to operationalize in terms of quality improvement. In order to improve quality, hospitals need clear rules regarding the patients to which it is attributed. While the authors compellingly argue that multiple-membership multilevel models do a better job mof measuring quality retrospectively than would be the case using HSAs alone, operationalizing the use of weighted HSANs in practice would be more difficult due to the model complexity. Nevertheless, this approach clearly highlights the challenges of using HAS-based catchment areas to measure quality of care.
Source:
- Falster, Michael O., Louisa R. Jorm, and Alastair H. Leyland. “Using Weighted Hospital Service Area Networks to Explore Variation in Preventable Hospitalization.” Health Services Research (2017).
Improving catchment area definitions when measuring quality of care posted first on http://ift.tt/2sNcj5z
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update
Last week, President Trump once again used the “M” word (“murder”) in a sentence accusing the pharmaceutical industry of too-high priced products for U.S. health citizens. The sentence included the phrase, “Drug companies are getting away with murder.” That week, USA Today published an article on a new FDA-approved specialty drug therapy that could add up to over a $1 mm price tag.
There is much to report in the world of pharmaceutical innovation, pricing, and patient Rx coverage this month. The CVS Health – Epic announcement ranks high in Health Populi’s vision for the evolving health/care ecosystem, bringing together two key industry leaders in their segments: retail pharmacy and prescription benefits management, and healthcare information technology. Each of these companies is the largest in their sector, and therefore brings scale and reach to this collaboration that aims to lower the cost of prescription drugs to plan members while bolstering medication adherence — two Holy Grails of healthcare in the current constrained health economy. The program has a strong population health focus, as well as a broad view on retail data to be included in the electronic health record: over-the-counter meds purchased in the “front of the store” will also be included in the patient’s EHR, allowing clinicians to have a more complete view of a person’s real-life medicines and supplements list.
On the drug-pricing front, PwC published its paper on Launching into Value, discussing pharma’s “quest” to align drug prices with outcomes. Broadly-defined, value has already come to health care and the concept will expand for both public payors (Medicare in 2018, and state Medicaid programs in various ways), and among commercial payors. Note that the Health Care Transformation Task Force, composed of major payors, purchasers, and patient advocacy groups, has committed to move 75% of the group’s collection business into value-based payment programs by 2020. PwC’s survey of pharmaceutical industry executives found that while the stakeholders are aware of value-based trends, only one-third of pharma execs believe the rewards of the programs align with the risks companies take in entering these contracts.
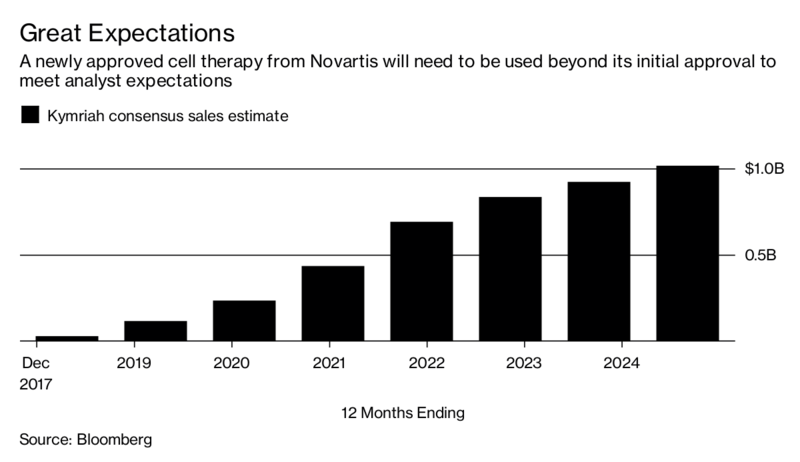 What is the value of a $1 mm therapy? That would be in the eye of the beholder: if you are a parent of a young child whose whole life potential lies ahead, $1 mm might look like a good deal. If you’re 75 in stage four of a painful cancel journey, then you might be at peace that life has been good, and enough. The CAR-T treatment branded as Kymriah was approved in August 2017 with a retail price of $475,000. An article in USA Today published last week estimated that the total cost of care under that therapy could reach $1.5 mm, based on the calculations of a leukemia specialist teaching at the University of Texas MD Anderson Cancer Center.
What is the value of a $1 mm therapy? That would be in the eye of the beholder: if you are a parent of a young child whose whole life potential lies ahead, $1 mm might look like a good deal. If you’re 75 in stage four of a painful cancel journey, then you might be at peace that life has been good, and enough. The CAR-T treatment branded as Kymriah was approved in August 2017 with a retail price of $475,000. An article in USA Today published last week estimated that the total cost of care under that therapy could reach $1.5 mm, based on the calculations of a leukemia specialist teaching at the University of Texas MD Anderson Cancer Center.
Now, to the question of affordability in the eyes of the patient. The Commonwealth Fund’s October 2017 issue brief asks the question, “How Well Does Insurance Coverage Protect Consumers From Health Care Costs?” analyzing the Fund’s biennial health insurance survey. I pulled the multi-colored bar chart which illustrates the reality that over two in five underinsured U.S. adults had problems getting healthcare due to cost. 28% of the underinsured did not fill a prescription due to cost.
The Foundation’s report discusses the Affordable Care Act’s positive outcome for gains in U.S. health citizens’ health care coverage and improvements on key indicators of access and reductions in medical bill problems. A study in this month’s Health Affairs has found that in California, peoples’ use of payday loans fell in concert with the expansion of Medicaid via the ACA, resulting in greater financial wellness for health citizens (in the short-term).
Health Populi’s Hot Points: The issue of “under-insurance” is timely given that the President, who has publicly spoken talked at least twice about the too-high cost of prescription drugs, has promoted the use of so-called skinny health plans that can fly under state regulatory radar. Thus the promise of innovative treatments such as CAR-T therapy for children diagnosed with acute lymphoblastic leukemia may just be a promise if pricing, and peoples’ ability to pay for new-and-improved medicines, do not align.
The post President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update appeared first on HealthPopuli.com.
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update posted first on http://ift.tt/2sNcj5z
Health plans getting into the PBM game
Bloomberg reports that Anthem is creating is own pharmacy benefits manager (PBM). Why? It says it wasn’t getting a good deal from PBMs.
Health insurer Anthem Inc. plans to set up its own pharmacy benefits management unit, signaling a final break with Express Scripts Holding Co. after accusing it of overcharging by billions of dollars.
The move means Express Scripts will not only lose its biggest client but also face a new rival. Anthem’s new unit, called IngenioRx, will grow its own business with a “full suite” of services, the insurer said in a statement on Wednesday.
How much was the overcharging? Anthem says the amount was $3 billion.
With drug prices on the rise, both pharma and PBM’s blame each other for high prices. PBMs say that drug list prices are too high. Pharmacetuical firms say they need to raise prices in order to offset large discounts and rebates that PBMs are demanding.
Anthem may not be the only firm entering the PBM market. Amazon is also considering entering the PBM market. UnitedHealth–Anthem’s top competitor–already has an in-house PBM known as OptumRx.
The one thing that is certain in the PBM world is that things are changing.
Health plans getting into the PBM game posted first on http://ift.tt/2sNcj5z
Quotation of the Day
To achieve greatness, two things are needed: a plan and not quite enough time
- Leonard Bernstein
Quotation of the Day posted first on http://ift.tt/2sNcj5z
Links
- 40% of American adults are obese.
- The real cost of drug development.
- Using the right p-value.
- The next big thing.
- Giannis!
Links posted first on http://ift.tt/2sNcj5z
CVS Health in Talks to Acquire Aetna – The Changing Retail Health Landscape
Just a few days since CVS Health announced the company would be working with mega-health insurer Anthem on a prescription drug management program, the pharmacy chain today is reportedly in talks to buy Aetna, the national health insurance company, according to CNBC and other credible news outlets like the Wall Street Journal.
Remember that Aetna’s bid to acquire Humana was scuttled earlier this year after many months of negotiation and positioning, along with FTC scrutiny about antitrust. That insurance merger “died” on one day in February 2017 along with an Anthem-CIGNA deal, covered here by CNN.
A deal between CVS Health and Aetna wouldn’t be subject to that kind of antitrust scrutiny given that this combination would be more of a vertical integration than horizontal expansion in the same industry, which the FTC worried would create monopoly power for insurance pricing in local/regional markets.
By vertically integrating, the CVS+Aetna entity could theoretically better manage healthcare costs through naturally bundling healthcare and pharmacy together, with incentives to manage patient care more holistically. This is certainly good positioning for addressing the Triple Aim and value-based payment that targets peoples’ health outcomes with lowering costs per capita.
Theoretically.
I’m writing this as a quick top-of-the mind announcement, and will do a deeper dive in tomorrow’s Health Populi.
For now, let the tectonic healthcare forces under our feet continue to rock and roll! As this growing retail health landscape is my wheelhouse, I’ll be wearing a proverbial helmet, knee pads, and other protective armaments as I try to forecast and analyze the ever-evolving health/care marketplace.
The post CVS Health in Talks to Acquire Aetna – The Changing Retail Health Landscape appeared first on HealthPopuli.com.
CVS Health in Talks to Acquire Aetna – The Changing Retail Health Landscape posted first on http://ift.tt/2sNcj5z
HWR is up
Health Wonk Review: Disaster edition is freshly posted by David Williams at the Health Business Blog. Check it out!
HWR is up posted first on http://ift.tt/2sNcj5z
In the Post-Weinstein Era, How to Market Health to Women: Philips, Kalenji, and Libresse Getting It Right
“With Mad Men still in charge, ad campaigns miss the mark,” an editorial published this week in the Financial Times asserts.
Leave it to a fiscally conservative British publication to be spot-on about a particularly, but not uniquely, American challenge, in this post-Weinstein (Miramax), -Price (Amazon), and today, -Halperin (MSNBC) moment of sexual harassment revelations.
In health/care, women are key consumers, buyers and influencers, yet under-represented in the Mad Men demographic of senior advertising executives, as the data-driven FT essay points out.
So it’s especially heartening to find this month a few examples of empowering, inspiring ad campaigns getting health/care marketing to women right.
Here is the video of Philip “Energía de madre” from Philips. I closely track Philips here on Health Populi in digital health, and discussed their expanded offerings for the connected baby and nursery after CES 2018 here. This month, if you live in Argentina, it was time to celebrate Mother’s Day. In this campaign, Philips is calling out las madres to celebrate their awesome energy. Adweek covered the video campaign, noting that, “The goal of the campaign was both to understand how much energy could be produced [by women living in and wearing connected shoes], and to find ways to reuse it for others. But ‘Mother’s Energy’ also highlights something else—the sheer work it takes to raise little humans.” As one mom says in the video, “That energy comes from love. Love for my children, for my family and for what I do as well.”
Check out Philips Better Me, Better World portal where you can see and share more examples of digital health goodness.
“Boobs are jealous of feet in a spot that promotes comfier sports bras,” AdAge described in another spot-on campaign promoting a new-and-improved brassiere from Kalenji. This spot leverages the fact that running for women impacts more than our feet, a fact long-overlooked by (male) shoe designers and ad makers. So this ad called “Jealous Boobs” brings some health literacy to the fore, with humor, joy, and great design sense. Little Black Book published some of the research data on this issue: specifically, breast movement increases up to 15 cm while running, and while most women experience breast pain when running, nearly one-half do not take action to alleviate their pain. The ad suggests that a good sports bra is a useful Rx for dealing with this real-life problem.
“Blood Normal,” the edgiest of my three ads comes from Libresse, a women’s health brand that markets tampons and other personal care products. Here’s the portal for the #BloodNormal campaign. According to Campaign (UK), Libresse’s corporate strategy focused on “breaking taboos that hold women back,” according to Martina Poulopoti, the global brand communication manager for parent company Essity. “We are hoping this positive representation of periods will help women and men all over the world understand that periods are normal, and that by showing them more and in a positive context we will start to break the taboos,” she was quoted to say.
To that end, here’s another ad from Libresse about “getting real” during a period.
Health Populi’s Hot Points: Let’s get real, Libresse-style, about a key point here: that these three ads were developed for audiences largely outside of the U.S. We’re way past a tipping point in America where the nation must get real about women’s health and healthcare, which includes our children’s, too. Gender health inequity still pervades U.S. healthcare treatment and outcomes. Women have paid more for healthcare, and for poorer outcomes, for decades. I talked about this recently in my Huffington Post column, “The Gender Disparity of Taxes, Toys, Tech and Tampons.”
This is not to say that men in the U.S. have perfect health and healthcare. Sadly, a segment of middle-aged American men have experienced an upturn in preventable mortality, too. But women’s health inequity in the U.S. is a long, old story, and particularly persistent for women of color.
Social determinants can/should go a long way to reducing health disparities, looking at income equality, transportation, food quality and security, safe and healthy housing. Health insurance security and health access (especially to evidence-based treatments, say, for heart disease), close this loop. These health-focused policies, baked into all public policy, can help to bend the cost-curve and flip disparities for both women and men, and for our kids.
In the meantime, I’m looking forward to “immigration” of these marketing ideas from outside the U.S. that educate, entertain, and empower women and their self-care. The health/care communications world may turn out to be flat, Thomas Friedman-style. With more women involved in all industries at senior levels, the day will come.
The post In the Post-Weinstein Era, How to Market Health to Women: Philips, Kalenji, and Libresse Getting It Right appeared first on HealthPopuli.com.
In the Post-Weinstein Era, How to Market Health to Women: Philips, Kalenji, and Libresse Getting It Right posted first on http://ift.tt/2sNcj5z
Wednesday, 25 October 2017
Health (Healthcare, Not So Much) Abounds in Prophet’s Top 50 Brands
U.S. consumers’ most-valued brands include Apple, Google, Amazon, Netflix, Pinterest, Android, Spotify, PIXAR, Disney and Samsung, according to the 2017 Brand Relevance Index from Prophet. The top 50 are shown in the first chart.
On the second chart, I’ve circled in red the brands that have reach into healthcare, health, fitness, and wellness. Arguably, I could have circled every brand in the top 50 because in one way or another, depending on the individual, people find health “everywhere” that’s relevant to them based on their own definitions and value-systems.
This is Prophet’s third year conducting this study, and I was keen to mine the health industry implications. I spent time on the phone with members of the team who work with the health industry and who have built this index from the beginning.
Prophet surveyed 13,500 U.S. consumers across 275 brands in 27 categories, using “4 Principles of Brand Relevance” in identifying consumers’ top relevant brands; they are,
- Customer obsessed (brands we can’t imagine living without)
- Ruthlessly pragmatic (brands we depend on)
- Distinctively inspired (brands that inspire us), and
- Pervasively innovative (brands that consistent innovate).
Traditional healthcare stakeholders – hospital systems, health plans, and insurers — don’t register highly in this study, Jeff Gourdji who leads health industry efforts at Prophet noted. This is because healthcare is generally a regional phenomenon. Thus, the “N” number of consumer respondents who named a particular healthcare organization is too small to compete with the likes of an Apple, Google, or Amazon.
Among all healthcare entities, the top-ranked brand this year was the Mayo Clinic. Other health system brands that bubbled up in the study included Cleveland Clinic, Northwestern Memorial, Dignity Health (which is a Health Populi brand favorite [not a client]), and Novant.
Health Populi’s Hot Points: There are indeed health/wellness/fitness brands in the Top 50, such as Crest (oral health), Dove (personal care), Fitbit (digital health), Under Armour (fitness and digital health), Nike (fitness), and adidas (fitness and digital health, and a client). Johnson & Johnson, #41 on the list, covers several segments in health and healthcare, including consumer/personal care, over-the-counter, medical devices, and pharmaceutical. J&J is the sole pharma in the Top 50, albeit probably not associated by consumers with the pharma aspects of the corporation. Note that Band-Aid, brand #36, is one of J&J’s consumer-facing products called out by consumers in the study.
There’s another lens through peoples’ “prismatic” perspectives on brands that suggest or enable health and wellness, Jesse Purewal, one of the innovators of this research, discussed. North Face’s branding invites us to never stop exploring, to be healthy living humans. Fitbit isn’t just a device but helps us achieve our personal goals. And, LEGO, I then riffed along, is one of my personal tools for mindfulness and fun – certainly health-building in the Kahn household of LEGOmaniacs.
Through my own Health-Is-Everywhere ecosystem perspective, I note in the second diagram just how many brands I see serving health and healthcare circled in red. Just ponder #1 Apple, #2 Google, #3 Amazon – three companies who have made significant health announcements in just the past few weeks. Others, like Samsung, Microsoft and SONY, are involved in health technology and medical devices. And in my expansive health/care-everywhere world, even Honda and Toyota, covered ten years ago here in Health Populi, are innovating in connected cars for the Internet-of-Health.
Many of my friends and colleagues would also name Hershey, brand #39, as a product for health when you just need that piece of dark chocolate to boost those flavonoids (which the Mayo Clinic discusses here).
Trader Joe’s, the top-ranked grocery brand in this study, can arguably through the lens of this health economist be a health destination for good food, sustainably sourced, at a good-value-for-money price, boosting financial wellness. This week, the Welltok consumer survey pointed out that financial stability is peoples’ top factor for health and wellness, further rationale for my assertion.
Patients, now health consumers, look to their favorite consumer-brands for health and wellbeing, along with value. Watch this space – it’s fast-growing and highly relevant to health consumers.
The post Health (Healthcare, Not So Much) Abounds in Prophet’s Top 50 Brands appeared first on HealthPopuli.com.
Health (Healthcare, Not So Much) Abounds in Prophet’s Top 50 Brands posted first on http://ift.tt/2sNcj5z
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep
THINK: money and love. To find health, working-aged people seek financial stability and good relationships, according to the Consumer Health POV Report from Welltok, meQuilibrium, and Zipongo, featured in their webinar broadcast today.
The online consumer survey was conducted among 2,000 full-time working U.S. adults in August 2017, segmented roughly into thirds by Boomers (37%), Gen Xers (32%), and Millennials (31%).
Much lower down the priority list for healthy living are managing food, sleep, and stress based on the poll.
Feeling stress is universal across most consumers in each of the three generational cohorts, especially related to work and finance.
While “manageable stress levels” comes in at a low 7% of respondents, it’s important to recognize the negative health and wellness impacts that financial instability and toxic relationships have on human health; these are bound up in the top two responses. For more evidence on that, turn to Christakis and Fowler’s research on being Connected — on the good and the bad aspects of our social networks.
For employers, the cost of stress is significant: 1 in 10 workers miss work due to stress, a study from the Faas Foundation and Mental Health America revealed this week. That cost adds up to some $500 bn a year for U.S. companies.
1 in 3 consumers felt the toll of stress, the report notes. Both men and women feel stress, with women more likely to feel “energy zapped” and appetites impacted (chocolate, anyone?). Connect that data point to the barriers to eating healthy by gender: women more often than men don’t have the time to buy and prepare healthy food, and also find eating healthy too expensive — a further stress related to finance.
Health Populi’s Hot Points: Financial wellness is integral to overall health and well-being. This was the theme of the first Health Populi blog post back in September 2007 – when health care was a top line-item in the national economy, taking a greater share out of peoples’ pockets. That was ten years ago, so it’s déjà vu…still. This photo from Tom’s Shell gas station illustrates what petrol-shopping drivers were perceiving at the time — that being asked to pay the price of gas in 2007 was akin to giving up your arm, leg, or first born.
It’s important to note that lower income Americans cared more about controlling or managing chronic health conditions versus consumers earning higher incomes, the survey found. That Welltok, meQuilibrium and Zipongo collaborated together in this study represents the kind of collaboration health consumers need industry stakeholders to forge to help people realize their holistic health goals.
Medical banking, data-collecting evidence-based beds, and health-personalized food kits: there is so much Blue Ocean to be filled based on consumer health-and-wellness wants. But through the economic lens of need vs. demand, where “demand” filters through peoples’ willingness-to-pay for products and services, which of these issues are high priorities for which consumers will pay hard dollars out-of-pocket?
This used to be the question I would ask before taking into account peoples’ now-holistic approach to personal and family health. More people, across social strata, are connecting the dots between their own determinants of health and health outcomes based on their personal values and sense of value — remember the survey finding that more lower-income people are trying to control chronic conditions compared with higher-income earners.
The grocery industry has certainly recognized this, with growing gluten-free aisles and pharmacies co-located with produce and center-store products. Pharmacies have blurred behind-the-counter with front-of-store, with more alliances being struck between food-and-pharmacy, and digital health as well. THINK: Walgreens Balance Rewards program (of which I am a beneficiary with many digital health trackers attached to the loyalty account, earning points every single day I wear them).
So the high-end bed becomes a health tool, and airlines are cutting deals with those bed companies to promote healthy sleep in the skies.
TD Bank gifted new deposit customers with Fitbit devices in sync with New Year’s Resolutions tying physical and fiscal fitness in January 2015. This is but one small tip of the iceberg of the New Retail Health. Stay tuned for more on this theme here in Health Populi, where on the advisory side of our work, we’re seeing new-new collaborations, products and services focused on this consumer-healthy sweet spot.
The post Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep appeared first on HealthPopuli.com.
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep posted first on http://ift.tt/2sNcj5z
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update
Last week, President Trump once again used the “M” word (“murder”) in a sentence accusing the pharmaceutical industry of too-high priced products for U.S. health citizens. The sentence included the phrase, “Drug companies are getting away with murder.” That week, USA Today published an article on a new FDA-approved specialty drug therapy that could add up to over a $1 mm price tag.
There is much to report in the world of pharmaceutical innovation, pricing, and patient Rx coverage this month. The CVS Health – Epic announcement ranks high in Health Populi’s vision for the evolving health/care ecosystem, bringing together two key industry leaders in their segments: retail pharmacy and prescription benefits management, and healthcare information technology. Each of these companies is the largest in their sector, and therefore brings scale and reach to this collaboration that aims to lower the cost of prescription drugs to plan members while bolstering medication adherence — two Holy Grails of healthcare in the current constrained health economy. The program has a strong population health focus, as well as a broad view on retail data to be included in the electronic health record: over-the-counter meds purchased in the “front of the store” will also be included in the patient’s EHR, allowing clinicians to have a more complete view of a person’s real-life medicines and supplements list.
On the drug-pricing front, PwC published its paper on Launching into Value, discussing pharma’s “quest” to align drug prices with outcomes. Broadly-defined, value has already come to health care and the concept will expand for both public payors (Medicare in 2018, and state Medicaid programs in various ways), and among commercial payors. Note that the Health Care Transformation Task Force, composed of major payors, purchasers, and patient advocacy groups, has committed to move 75% of the group’s collection business into value-based payment programs by 2020. PwC’s survey of pharmaceutical industry executives found that while the stakeholders are aware of value-based trends, only one-third of pharma execs believe the rewards of the programs align with the risks companies take in entering these contracts.
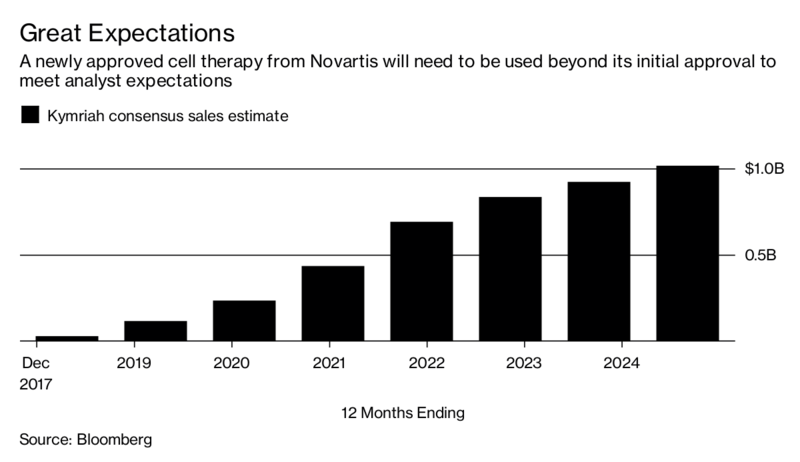 What is the value of a $1 mm therapy? That would be in the eye of the beholder: if you are a parent of a young child whose whole life potential lies ahead, $1 mm might look like a good deal. If you’re 75 in stage four of a painful cancel journey, then you might be at peace that life has been good, and enough. The CAR-T treatment branded as Kymriah was approved in August 2017 with a retail price of $475,000. An article in USA Today published last week estimated that the total cost of care under that therapy could reach $1.5 mm, based on the calculations of a leukemia specialist teaching at the University of Texas MD Anderson Cancer Center.
What is the value of a $1 mm therapy? That would be in the eye of the beholder: if you are a parent of a young child whose whole life potential lies ahead, $1 mm might look like a good deal. If you’re 75 in stage four of a painful cancel journey, then you might be at peace that life has been good, and enough. The CAR-T treatment branded as Kymriah was approved in August 2017 with a retail price of $475,000. An article in USA Today published last week estimated that the total cost of care under that therapy could reach $1.5 mm, based on the calculations of a leukemia specialist teaching at the University of Texas MD Anderson Cancer Center.
Now, to the question of affordability in the eyes of the patient. The Commonwealth Fund’s October 2017 issue brief asks the question, “How Well Does Insurance Coverage Protect Consumers From Health Care Costs?” analyzing the Fund’s biennial health insurance survey. I pulled the multi-colored bar chart which illustrates the reality that over two in five underinsured U.S. adults had problems getting healthcare due to cost. 28% of the underinsured did not fill a prescription due to cost.
The Foundation’s report discusses the Affordable Care Act’s positive outcome for gains in U.S. health citizens’ health care coverage and improvements on key indicators of access and reductions in medical bill problems. A study in this month’s Health Affairs has found that in California, peoples’ use of payday loans fell in concert with the expansion of Medicaid via the ACA, resulting in greater financial wellness for health citizens (in the short-term).
Health Populi’s Hot Points: The issue of “under-insurance” is timely given that the President, who has publicly spoken talked at least twice about the too-high cost of prescription drugs, has promoted the use of so-called skinny health plans that can fly under state regulatory radar. Thus the promise of innovative treatments such as CAR-T therapy for children diagnosed with acute lymphoblastic leukemia may just be a promise if pricing, and peoples’ ability to pay for new-and-improved medicines, do not align.
The post President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update appeared first on HealthPopuli.com.
President Trump Utters “M” for Murder, and a $1 MM Price Tag for Rx Therapy – an October 2017 Pharma Update posted first on http://ift.tt/2sNcj5z
Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare
Old-age inequality among current retirees in the U.S. is already greater than in ever OECD country except Chile and Mexico, revealed in Preventing Ageing Unequally from the OECD.
Key findings from the report are that:
- Inequalities in education, health, employment and income start building up from early ages
- At all ages, people in bad health work less and earn less. Over a career, bad health reduces lifetime earnings of low-educated men by 33%, while the loss is only 17% for highly-educated men
- Gender inequality in old age, however, is likely to remain substantial: annual pension payments to the over-65s today are about 27% lower for women on average, and old-age poverty is much higher among women than men.
For economists, income inequality is expressed as the Gini coefficient: the greater the value of the Gini coefficient, the higher the inequality in a nation. In the U.S., the Gini coefficient has been rising from one American generation to the next since 1920, shown in the second chart.
Health problems are a big reason contributing to increasing inequality. Americans are unhealthier than health citizens in other countries, particularly people earning lower incomes. “Disabilities, depression and obesity are widespread” in this group of people, the OECD observes. Over 1 in 3 Americans is obese, more than in any other OECD country.
To address this challenge, OECD offers three recommendations:
Prevent inequality before it grows over time, providing good childcare, early childhood education, cover healthcare early in a person’s life, and expanding youth work opportunities
Mitigate inequalities when they arise, through job services to get unemployed people back to work, targeting population health programs, and hiring older workers
Cope with older-age inequalities, like addressing women’s pension adequacy, ensuring affordable quality home care, and providing support for caregivers who perform high-value tasks for little to no economic benefit.
Here is a link to the OECD’s US report on income inequality in aging.
Health Populi’s Hot Points: “Health problems and employment disadvantages reinforce each other,” leading to more unhealthy poorer people, OECD warns. Policies can address the challenge of getting and keeping people healthy and in employment as long as possible, which boosts retirement incomes and mitigates poverty risks and “unequal aging.”
At this very moment, for example, the Children’s Health Insurance Program has yet to be re-authorized by the U.S. Congress. This program, founded in a bi-partisan way by Senators Edward Kennedy (Democrat) and Orrin Hatch (Republican), ensures that kids in America get access to health care — the kind of basic healthcare that the OECD asserts helps to prepare a citizenry for education and work, to contribute to society as full members (and taxpayers).
Other public policies can be designed to “bake” health into them, from food and transportation to housing and environmental standards. All of these social determinants influence health from birth.
Digital technologies can also help to support people’s social and health care in aging, and can address disparities and gaps in care. Dr. Joe Kvedar’s new book features innovations on the Internet of Healthy Things for aging and longevity. Remote health monitoring is gaining clinical-economic evidence to support people managing chronic conditions to live and age well at home, not in institutions — bringing down the total cost of care over the life-cycle and also enhance quality of life in one’s beloved surroundings. Intel’s announcement today in partnership with Flex in development of a Health Application Platform addresses this market, especially for remote health monitoring and the HealthIoT [I’ll be posting more on that in tomorrow’s Health Populi].
See Laurie Orlov’s Aging in Place Technology Watch, published, yesterday on the importance of “monitoring the person AND the place.” Here is her last paragraph which nails the design challenge:
“How about monitoring person and the place? While each solution categories by itself may useful, each is incomplete. On the body technologies should link to on-the-server hubs of useful health information for families and providers. In the (patient and care recipient) rooms, add the up-and-about wearables capturing and serving data that can follow the discharged patients into their homes and connect with any sensors placed there. Anomalies of behavior like falling or lack of motion are essential. Printed discharge instructions must be replaced with voice-first technologies that answer a person’s key questions: “Which pills am I supposed to take with food?” “What should I do if my heart starts skipping beats?” “When is the ride pickup for my follow-up appointment?” “Please ask my son to call me – now.” We’re not there yet in terms of what older adults need – and it’s not for lack of technology. And it is a shame.”
Here’s a great infographic published in concert with the Connected Health Conference, Dr. Kvedar’s longtime meet-up addressing digital health, now part of HIMSS and the Personal Connected Health Alliance.
The post Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare appeared first on HealthPopuli.com.
Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare posted first on http://ift.tt/2sNcj5z
How much is your life worth?
According to the Environmental Protection Agency, the answer is $10 million. Other agencies place use a somewhat lower number. The Food and Drug administration pegs the value at $9.5 million and the Department of Agriculture places the value at $8.9 million.
Technically, what these agencies are calculating are the value of a statistical life (VSL). Although measuring the value of a life is an interesting academic exercise, it has real world implications. Notably, VSL is used in federal agencies cost benefit analyses.
For instance, consider a new regulation to reduce pollution that saves 10 lives but costs $50 million. Should society undertake this intervention? If VSL is $10 million, then the answer is ‘yes.’ Each of the 10 lives is worth $10 million so the regulation leads to $100 million in benefits but only costs $50 million.
On the other hand, consider a more drastic intervention for reducing population: making privately owned cars illegal. In this case, let us say the intervention saved 10 lives still but the cost now is $1 billion is lost economic activity. In this second example, the costs outweigh the benefits and so based pursed on aggregated costs and benefits, we would not implement this intervention.
For the politically minded, those who prefer more regulation would prefer a higher VSL and those who prefer less regulaion would opt for a lower VSL.
How much is your life worth? posted first on http://ift.tt/2sNcj5z
Tuesday, 24 October 2017
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep
THINK: money and love. To find health, working-aged people seek financial stability and good relationships, according to the Consumer Health POV Report from Welltok, meQuilibrium, and Zipongo, featured in their webinar broadcast today.
The online consumer survey was conducted among 2,000 full-time working U.S. adults in August 2017, segmented roughly into thirds by Boomers (37%), Gen Xers (32%), and Millennials (31%).
Much lower down the priority list for healthy living are managing food, sleep, and stress based on the poll.
Feeling stress is universal across most consumers in each of the three generational cohorts, especially related to work and finance.
While “manageable stress levels” comes in at a low 7% of respondents, it’s important to recognize the negative health and wellness impacts that financial instability and toxic relationships have on human health; these are bound up in the top two responses. For more evidence on that, turn to Christakis and Fowler’s research on being Connected — on the good and the bad aspects of our social networks.
For employers, the cost of stress is significant: 1 in 10 workers miss work due to stress, a study from the Faas Foundation and Mental Health America revealed this week. That cost adds up to some $500 bn a year for U.S. companies.
1 in 3 consumers felt the toll of stress, the report notes. Both men and women feel stress, with women more likely to feel “energy zapped” and appetites impacted (chocolate, anyone?). Connect that data point to the barriers to eating healthy by gender: women more often than men don’t have the time to buy and prepare healthy food, and also find eating healthy too expensive — a further stress related to finance.
Health Populi’s Hot Points: Financial wellness is integral to overall health and well-being. This was the theme of the first Health Populi blog post back in September 2007 – when health care was a top line-item in the national economy, taking a greater share out of peoples’ pockets. That was ten years ago, so it’s déjà vu…still. This photo from Tom’s Shell gas station illustrates what petrol-shopping drivers were perceiving at the time — that being asked to pay the price of gas in 2007 was akin to giving up your arm, leg, or first born.
It’s important to note that lower income Americans cared more about controlling or managing chronic health conditions versus consumers earning higher incomes, the survey found. That Welltok, meQuilibrium and Zipongo collaborated together in this study represents the kind of collaboration health consumers need industry stakeholders to forge to help people realize their holistic health goals.
Medical banking, data-collecting evidence-based beds, and health-personalized food kits: there is so much Blue Ocean to be filled based on consumer health-and-wellness wants. But through the economic lens of need vs. demand, where “demand” filters through peoples’ willingness-to-pay for products and services, which of these issues are high priorities for which consumers will pay hard dollars out-of-pocket?
This used to be the question I would ask before taking into account peoples’ now-holistic approach to personal and family health. More people, across social strata, are connecting the dots between their own determinants of health and health outcomes based on their personal values and sense of value — remember the survey finding that more lower-income people are trying to control chronic conditions compared with higher-income earners.
The grocery industry has certainly recognized this, with growing gluten-free aisles and pharmacies co-located with produce and center-store products. Pharmacies have blurred behind-the-counter with front-of-store, with more alliances being struck between food-and-pharmacy, and digital health as well. THINK: Walgreens Balance Rewards program (of which I am a beneficiary with many digital health trackers attached to the loyalty account, earning points every single day I wear them).
So the high-end bed becomes a health tool, and airlines are cutting deals with those bed companies to promote healthy sleep in the skies.
TD Bank gifted new deposit customers with Fitbit devices in sync with New Year’s Resolutions tying physical and fiscal fitness in January 2015. This is but one small tip of the iceberg of the New Retail Health. Stay tuned for more on this theme here in Health Populi, where on the advisory side of our work, we’re seeing new-new collaborations, products and services focused on this consumer-healthy sweet spot.
The post Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep appeared first on HealthPopuli.com.
Four Things We Want in 2017: Financial Health, Relationships, Good Food, and Sleep posted first on http://ift.tt/2sNcj5z
Oral Cancer in Men Caused by Sexually Transmitted Virus Is on the Rise
Not long ago, the prevention and treatment of deadly cancers linked to the sexually transmitted human papillomavirus (HPV) was thought to be mainly a women’s health issue. While HPV-linked cancers were known to affect people of either sex, the number-one cause of mortality from HPV infection was cervical cancer. But a recent study in the journal Annals of Internal Medicine should serve as a loud wakeup call to sexually active men: The incidence of oral cancers in men caused by HPV is now surpassing that of cervical cancer in women.
According to the study, some 11 million men in the United States have oral HPV infections, as opposed to 3.2 million women. Higher-risk strains of the virus, which can cause cancers of mouth, tongue and throat, were present in 7.3% of men and 1.4% of women. HPV can be passed from person to person by intercourse as well as oral sex. And one particularly troublesome strain, HPV-16, is six times more common in men than in women.
In the past, medical professionals regarded tobacco use and alcohol consumption as the main risk factors for oral cancer. But today, the fastest-growing group of new oral cancer patients is young people of either sex, who are infected by sexually transmitted strains of the HPV virus. And that’s something we all need to learn more about.
At Dear Doctor, we have been following this disturbing trend for some time. In recent issues of Dear Doctor–Dentistry & Oral Health magazine, we mourned the loss of legendary slugger Tony Gwinn to oral cancer; presented a cancer survivor’s story; and previewed a new salivary test that could help identify people who need a biopsy. We have also emphasized the importance of routine dental exams in diagnosing and treating diseases like oral cancer—and in many cases, even preventing those diseases.
So let’s take this opportunity to review what you can do to fight oral cancer. First, practicing safer sex is important; it can help protect you from HPV and other diseases as well. Avoid overuse of alcohol and quit using tobacco of any type—including smokeless “dip.” Next, become more informed about oral cancer, including its causes, symptoms, prevention and treatment. (The articles on deardoctor.com are a great place to start.) Learn how to perform a self-exam for oral cancer—and make sure to get regular dental checkups, where your dentist can perform a thorough oral cancer screening. Finally, ask your health care provider about the HPV vaccine (Parents: that goes for boys as well as girls).
Oral cancer may be a scary thing to talk about—but it’s a conversation many of us need to have. The good news is that when oral cancer is found and managed early, the odds of successful treatment go way up.
Oral Cancer in Men Caused by Sexually Transmitted Virus Is on the Rise posted first on http://ift.tt/2sNcj5z
Improving catchment area definitions when measuring quality of care
Oftentimes, we want to measure the quality of care of a give hospital or health care system. The easiest way of doing this is to measure the quality of care received by patients who go to that hospital. These patients, however, may attend multiple hospitals during they year. Further, if quality of care includes avoiding hospitalizations, we need to identify not only patients who had a hospital admission but patients who were at risk of going to that hospital if a preventable admission occurred.
One way to model quality of care is to use catchment areas. Catchment areas are typically aggregations of geographic units. For instance, hospital service areas (HSAs) are aggregations of ZIP codes. However, previous research has shown that HSA-based catchment areas only capturing 50% to 80% of hospital admissions for their given population. One could use larger geographic regions—such as hospital referral regions (HRRs)—but then one is susceptible to assigning patients to hospitals over which they are unlikely to have responsibility for their care.
My previous research on the hospital wage index (see here and here) proposed assigning a weighting of the geographic units While that approach aimed to measure geographic variation in wages where data was available by geography rather than by person, an interesting paper by Falster, Jorn and Leyland (2017) proposes a different approach using individual patient data and a methodology known as multiple-membership multi-level model multi-level.
To explain this model, consider first a standard approach whereby where I people are clustered within J hospitals or HSAs.
Yij is the outcome, xpi are the regression parameters for P person-level variables, and xqj are the regression parameters for Q hospital-level variables. This multilevel model captures the effects of clustering by allowing both regression parameters and error terms to exist at different hierarchical levels.
A multiple-membership multilevel model extends this approach by allowing a weighted structure for each of the hospital-level components as follows:
Here, the superscripts represent the different model hierarchy levels. Faster and co-authors apply this model to date on preventable hospitalizations in NSW Australia using weighted hospital service area networks (weighted-HSANs). The authors contend that:
Between-hospital variation in rates of preventable hospitalization was more than two times greater when modeled using weighted-HSANs rather than HSAs. Use of weighted-HSANs permitted identification of small hospitals with particularly high rates of admission and influenced performance ranking of hospitals, particularly those with a broadly distributed patient base.
While this approach is a significant improvement for an academic setting, it is problematic to operationalize in terms of quality improvement. In order to improve quality, hospitals need clear rules regarding the patients to which it is attributed. While the authors compellingly argue that multiple-membership multilevel models do a better job mof measuring quality retrospectively than would be the case using HSAs alone, operationalizing the use of weighted HSANs in practice would be more difficult due to the model complexity. Nevertheless, this approach clearly highlights the challenges of using HAS-based catchment areas to measure quality of care.
Source:
- Falster, Michael O., Louisa R. Jorm, and Alastair H. Leyland. “Using Weighted Hospital Service Area Networks to Explore Variation in Preventable Hospitalization.” Health Services Research (2017).
Improving catchment area definitions when measuring quality of care posted first on http://ift.tt/2sNcj5z